Rest Easy: How CBT-I Can Transform Your Sleep

Still Awake at 2AM? Here’s the Real Reason You Can’t Sleep (and How CBT for Insomnia Can Fix It)
CBT for insomnia (CBT-I) is a structured, evidence-based therapy that targets the thoughts, behaviors, and habits keeping you awake—helping 70-80% of people with chronic insomnia sleep better without medication.
Quick Answer for “CBT for Insomnia”:
- What it is: A 6-8 session program that fixes the root causes of insomnia
- How it works: Changes negative sleep thoughts, retrains your brain to associate bed with sleep, and builds healthy sleep habits
- Results: Most people improve in 4-6 sessions; effects last 2+ years
- Who it helps: Adults with chronic or short-term insomnia—even with anxiety, depression, or other conditions
- First-line treatment: Recommended by the American College of Physicians over sleeping pills
You’ve tried everything. Sleep hygiene tips. Melatonin. Counting sheep. Maybe even prescription pills that left you groggy the next day. But night after night, you’re still staring at the ceiling at 2AM, dreading the alarm that’s only hours away.
Chronic insomnia isn’t just annoying—it’s dangerous. It wrecks your focus, tanks your mood, weakens your immune system, and raises your risk for serious health problems like heart disease and depression. And you’re not alone: 6-10% of adults struggle with chronic insomnia, tossing and turning while the rest of the world sleeps.
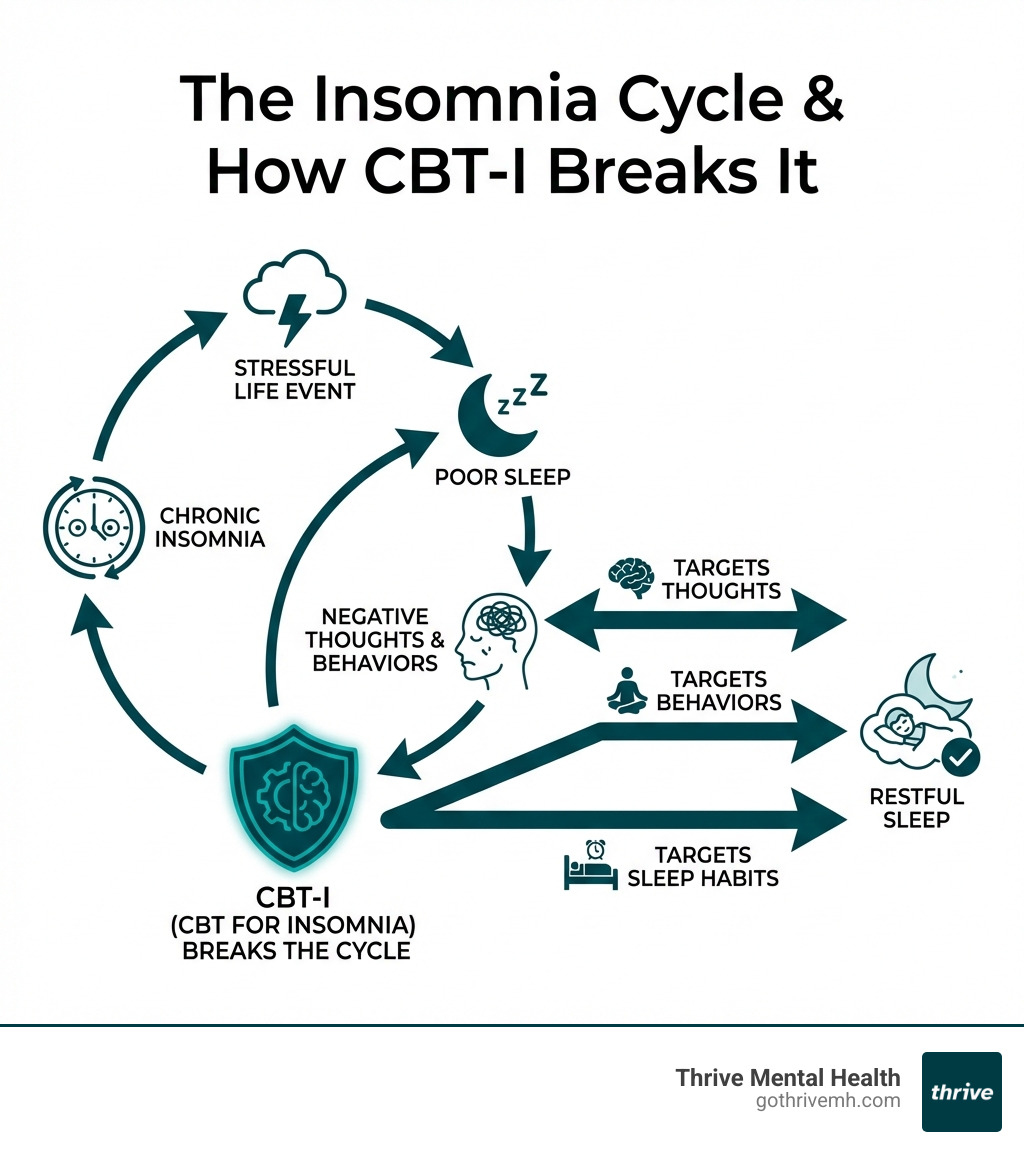
Most people think insomnia is just “bad sleep.” But it’s actually a cycle—stress triggers poor sleep, which fuels anxious thoughts, which creates bad habits, which keeps you awake. Pills might knock you out temporarily, but they don’t fix the cycle. That’s why the American College of Physicians recommends CBT for insomnia as the first-line treatment—not medication.
CBT-I works because it targets what’s actually keeping you awake: negative conditioning, racing thoughts, and poor sleep routines. It’s fast (most people see results in 4-6 sessions), safe (no side effects or dependency), and lasting (benefits stick around for 2+ years). And unlike pills, it teaches you skills you’ll use for life.
I’m Nate Raine, CEO of Thrive Mental Health, and I’ve spent over a decade building evidence-based behavioral health programs that deliver real, measurable outcomes. At Thrive, we use CBT for insomnia as part of our integrated approach to mental health, helping clients across Florida finally break the cycle and sleep through the night.
Handy cbt for insomnia terms:
What Is CBT for Insomnia? Why Experts Say It’s the Fastest, Safest Fix
Cognitive Behavioral Therapy for Insomnia (CBT-I) is a highly structured, multi-component treatment designed to help you overcome chronic sleeplessness. It’s not just a set of tips; it’s a therapeutic process that retrains your brain and body for healthy sleep. We understand that battling insomnia can feel isolating and frustrating, but with CBT-I, we offer a proven path to lasting relief.
Why is CBT-I considered the gold standard? Because it addresses the core issues that keep you awake. Insomnia isn’t usually caused by a single factor, but rather a complex interplay of predisposing factors (like a genetic tendency towards light sleep), precipitating factors (like a stressful life event), and crucially, perpetuating factors. These perpetuating factors are the unhelpful thoughts, beliefs, and behaviors that develop in response to initial sleep problems and then keep the insomnia going long after the initial trigger is gone. CBT-I specifically targets these perpetuating factors, breaking the cycle and restoring your natural ability to sleep.
The statistics speak for themselves:
- 6–10% of adults have chronic insomnia, making it the most prevalent sleep disorder.
- 70–80% of patients with primary insomnia experience significant improvements when using multicomponent CBT-I techniques. This means less time to fall asleep, more time spent asleep, and fewer awakenings during the night.
- Results last up to 2 years or more. Unlike sleeping pills, which offer temporary relief, CBT-I equips you with skills for long-term sleep health. Clinical gains can be maintained for up to 24 months post-treatment.
- It’s effective for both short-term and chronic insomnia. Whether your sleepless nights are recent or have plagued you for years, CBT-I provides a powerful solution.
- The American College of Physicians recommends CBT-I as the first-line approach for all adult patients with chronic insomnia. This powerful endorsement highlights its superior long-term efficacy and safety compared to pharmacological treatments.
At Thrive Mental Health, our virtual and in-person programs are designed to deliver this transformative treatment. We believe in providing access to evidence-based care that truly works, and CBT for insomnia is a cornerstone of that commitment.
Internal link: Learn more about Thrive’s Virtual Therapy and IOP programs.
How CBT for Insomnia Works: The 4 Steps That Rewire Your Brain for Sleep
Insomnia isn’t just “bad sleep”—it’s a cycle of habits, thoughts, and stress. Think of it like this: when you first start having trouble sleeping, you might develop new habits or ways of thinking in an attempt to “fix” it. Unfortunately, these coping mechanisms often make the problem worse, leading to a conditioned response where your bed, or even the thought of sleep, becomes a trigger for wakefulness and anxiety.
CBT-I breaks this cycle by addressing these conditioned responses and replacing them with healthy, sleep-promoting patterns. We work together to identify and change the specific thoughts and behaviors that are sabotaging your sleep, helping you regain control and trust in your body’s natural ability to rest.

The core components of CBT for insomnia include a mix of behavioral interventions, cognitive restructuring, and psychoeducation. Let’s explore the key steps:
1. Stimulus Control: Re-Train Your Brain to Sleep in Bed
Imagine your bed as a sacred space, reserved exclusively for sleep and intimacy. For many people with insomnia, the bed becomes associated with frustration, anxiety, and wakefulness because they spend too much time there doing non-sleep activities. Stimulus Control Therapy (SCT) aims to break this negative association and re-establish your bed and bedroom as strong cues for sleep.
Here’s how we typically implement it:
- Only use your bed for sleep and sex. This means no reading, watching TV, working, eating, or scrolling on your phone while in bed. If you need to do these activities, do them in another room.
- If you can’t sleep within 20 minutes, get up. Lying in bed awake only reinforces the connection between your bed and wakefulness. Get out of bed, go to another room, and engage in a calm, non-stimulating activity (like reading a boring book under dim light) until you feel genuinely sleepy. Only then should you return to bed. Repeat this as many times as necessary throughout the night.
- Wake up at the same time every day—even weekends. This is one of the most crucial components. A consistent wake-up time helps regulate your body’s natural sleep-wake cycle (circadian rhythm), making it easier to fall asleep at night.
This might sound challenging, especially at first, but by consistently following these rules, you’ll gradually re-associate your bed with quick, efficient sleep. It’s about teaching your brain that the bed is for sleeping, and nothing else.
Internal link: See how Thrive’s behavioral therapy helps you break bad sleep habits.
2. Sleep Restriction: Build Real Sleep Drive (Not Just “More Time in Bed”)
This component often raises eyebrows, but it’s incredibly effective. Sleep Restriction Therapy (SRT) might seem counterintuitive because it involves intentionally limiting the amount of time you spend in bed. The goal isn’t to deprive you of sleep, but to increase your body’s natural “sleep drive” (homeostatic sleep drive) and make your sleep more consolidated and efficient.
Here’s the process:
- Limit time in bed to match your actual sleep time. We start by having you keep a detailed sleep diary for 1-2 weeks. This helps us determine your average actual sleep duration. Then, we set your “prescribed time in bed” (PTIB) to roughly match that average. For example, if you’re spending 8 hours in bed but only getting 5 hours of sleep, we might initially restrict your time in bed to 5.5 hours. This creates a mild sleep deprivation that makes you fall asleep faster and stay asleep longer during your limited sleep window.
- Track your sleep with a diary. Consistent tracking is essential. You’ll record when you go to bed, when you fall asleep, how many times you wake up, when you wake up for good, and your overall sleep quality. This data allows your therapist to make informed adjustments.
- Gradually increase time in bed as your sleep improves. Once your sleep becomes more efficient (meaning you’re spending most of your restricted time in bed actually sleeping), we’ll slowly increase your time in bed by 15-30 minute increments. This continues until you’re sleeping well and getting an adequate amount of sleep, typically 7-8 hours for most adults. Sleep compression is a gentler version of this, gradually reducing time in bed rather than a sharp restriction, which can be useful for some individuals.
While the initial phase of sleep restriction can lead to temporary fatigue, the long-term benefits of consolidated, high-quality sleep far outweigh this temporary discomfort. It’s a powerful way to reset your sleep system.
3. Change Your Thoughts: Stop the “I’ll Never Sleep” Spiral
Insomnia isn’t just a physical problem; it’s deeply intertwined with your mind. Many people with chronic insomnia develop negative, unhelpful, or even catastrophic thoughts and beliefs about sleep. Thoughts like “I’ll never fall asleep,” “I can’t function tomorrow if I don’t get 8 hours,” or “This sleeplessness is ruining my life” can create significant anxiety and arousal, making sleep impossible.
Cognitive Therapy (CT) helps you identify and challenge these dysfunctional thoughts and beliefs. We work on:
- Spotting and challenging negative beliefs. We’ll help you recognize these automatic negative thoughts (ANTs) as they arise. For example, if you think, “I’ll be a wreck tomorrow,” we’ll explore the evidence for and against that thought. Are you always a wreck? What have you managed to do on little sleep before?
- Replacing catastrophic thinking with facts. Instead of focusing on worst-case scenarios, we guide you to develop more balanced and realistic perspectives. For instance, realizing that while sleep deprivation is unpleasant, one poor night won’t cause irreversible damage. The ability to “let go” and observe thoughts non-judgmentally, rather than engaging with them, is a key skill taught in this component.
- Using thought records to reduce sleep anxiety. This involves documenting your thoughts, the emotions they trigger, and then actively re-evaluating and reframing them. This process helps reduce the emotional distress associated with sleeplessness, which is a significant perpetuating factor of insomnia.
By changing the way you think about sleep, you can reduce the anxiety that keeps you awake and foster a more positive, relaxed mindset conducive to rest.
4. Sleep Hygiene & Relaxation: Set Up Your Night for Success
While often not enough on its own to cure chronic insomnia, good sleep hygiene forms the foundation of healthy sleep and is an integral part of CBT-I. It involves establishing daily practices and environmental conditions that promote consistent, restorative sleep. Alongside this, relaxation techniques help calm your mind and body, preparing you for rest.
Here’s a list of key sleep hygiene rules and relaxation techniques we emphasize:
- Keep your bedroom cool, dark, and quiet. Your sleep environment plays a huge role. Aim for a room temperature between 60-67 degrees Fahrenheit (15-19 degrees Celsius). Block out light with blackout curtains and minimize noise with earplugs or a white noise machine.
- Avoid caffeine after 2PM. Caffeine is a stimulant that can stay in your system for hours, disrupting sleep.
- No heavy meals or alcohol before bed. Heavy meals can cause digestive discomfort, while alcohol, though initially sedating, fragments sleep later in the night and can worsen snoring.
- Exercise regularly—but not right before sleep. Regular physical activity promotes better sleep, but intense exercise too close to bedtime can be stimulating. Aim to finish vigorous workouts at least a few hours before bed.
- Create a consistent, relaxing nightly routine. This signals to your body that it’s time to wind down. This could include a warm bath, reading (not on a screen), gentle stretching, or listening to calm music.
- Limit exposure to bright light (especially blue light) in the evening. Screens from phones, tablets, and computers emit blue light that can interfere with melatonin production, a hormone essential for sleep.
- Expose yourself to bright light in the morning. This helps reinforce your natural circadian rhythm.
Try relaxation techniques: These help reduce pre-sleep arousal and anxiety. We might guide you through:
- Deep breathing exercises: Slow, diaphragmatic breathing can activate your parasympathetic nervous system, promoting relaxation.
- Progressive Muscle Relaxation (PMR): Tensing and then releasing different muscle groups throughout your body helps you become aware of physical tension and release it.
- Guided imagery or meditation: Focusing on calming mental images or practicing mindfulness can quiet a racing mind.
- Biofeedback: Learning to control physiological responses like heart rate or muscle tension can be an effective way to promote relaxation.
By integrating these practices into your daily life, you create an optimal environment and mindset for falling asleep and staying asleep.
CBT for Insomnia vs. Sleeping Pills: What You Need to Know [TABLE]
For years, sleeping pills were the go-to solution for insomnia. While they can provide quick, short-term relief, they come with significant drawbacks that CBT-I largely avoids. We believe in empowering you with sustainable solutions, not temporary fixes that can lead to dependency.
Here’s a clear comparison:
| Feature | CBT for Insomnia (CBT-I) | Sleeping Pills (Hypnotics) |
|---|---|---|
| Effectiveness | Highly effective for chronic insomnia (70-80% improvement). Comparable to pills in short-term; superior long-term. | Effective for short-term symptom relief. |
| Side Effects | Minimal; may include temporary fatigue during initial sleep restriction. | Can cause grogginess, dizziness, impaired coordination, memory issues, dependence, rebound insomnia. |
| Long-Term Results | Durable, lasting effects (2+ years). Teaches coping skills for life. | Effects diminish over time; often require increasing doses. |
| Dependency Risk | None. Focuses on natural sleep mechanisms. | High risk of psychological and physiological dependence. |
| Mechanism | Addresses underlying thoughts, behaviors, and conditioning. | Masks symptoms by inducing sedation. |
| Cost-Effectiveness | Higher upfront investment, but long-term savings from reduced medication use and improved health. | Lower initial cost, but ongoing expense and potential for higher healthcare costs due to side effects. |
| Safety | Very safe; no risk of overdose or dangerous interactions. | Can be dangerous, especially with alcohol or other medications. |
| Relapse Rate | Lower relapse rates due to learned coping skills. | Higher relapse rates once medication is stopped. |
Sleeping pills might offer a quick fix, especially if you’re experiencing acute insomnia due to a major stressor. However, for chronic insomnia, they are generally not the best long-term solution. Many medical conditions and mental health conditions can disrupt sleep, and it’s unlikely that all insomnia symptoms will go away with medicines alone. The potential for dependence, withdrawal symptoms, memory issues, and daytime grogginess makes them a less desirable option for sustainable sleep health.
CBT for insomnia delivers lasting results—no withdrawal, no next-day fog. It helps you understand and manage the root causes of your sleep problems, giving you the tools to sleep well for years to come. This empowerment is a key benefit we see in our clients at Thrive Mental Health.
Internal link: Compare Thrive’s IOP and PHP programs for sleep and mental health.
Who Can Benefit from CBT-I?
CBT for insomnia is a versatile and highly effective treatment for a wide range of individuals struggling with sleep. If you’re an adult experiencing chronic insomnia—meaning difficulty falling or staying asleep, or waking too early, for at least three nights a week for three months or more—CBT-I is likely an excellent option for you.
But its benefits extend far beyond primary insomnia. CBT-I is effective even if your sleep problems are linked to other health conditions. This includes individuals with:
- Anxiety and depression: Insomnia often co-occurs with mood disorders. CBT-I can improve sleep, which in turn can significantly reduce symptoms of anxiety and depression.
- Chronic pain: Managing pain can be exhausting, and poor sleep often exacerbates pain. CBT-I helps break this vicious cycle.
- Post-Traumatic Stress Disorder (PTSD): Sleep disturbances, including nightmares, are common in PTSD. CBT-I, sometimes combined with imagery rehearsal therapy, can be highly beneficial.
- Other medical conditions: People with conditions like cancer, HIV, or heart disease often experience sleep difficulties, and CBT-I can provide much-needed relief.
- Pregnancy: Hormonal changes and discomfort can lead to insomnia during pregnancy, and CBT-I offers a safe, non-pharmacological approach.
Essentially, if you’re tired of being tired and are looking for a sustainable, evidence-based solution that empowers you with long-term skills, CBT for insomnia could be the game-changer you need. It teaches you how to be your own sleep expert.
What to Expect: Your CBT for Insomnia Program at Thrive
Starting on a CBT for insomnia program at Thrive Mental Health means choosing a path to sustainable sleep health. We understand that starting therapy can feel like a big step, and we’re here to guide you through every stage with expertise and compassion.
Our programs are built on flexibility and personalized care, designed to integrate seamlessly into your life. Here’s what you can generally expect:
- Most people see big changes in 4–8 sessions. While some individuals experience significant improvements after just two sessions, the standard treatment is typically delivered over six to eight sessions. This structured approach allows for gradual implementation of techniques and consistent monitoring of progress. The average treatment effect sizes are impressive, corresponding to approximately a 50% post-treatment reduction in individual insomnia symptoms.
- You’ll work with a licensed therapist, in-person or virtually, with flexible scheduling. Our team comprises experienced and credentialed behavioral sleep medicine specialists. We offer individual therapy sessions, and for those who benefit from shared experiences and peer support, we also facilitate virtual group therapy sessions. Our flexible scheduling, including evening and weekend options, is designed to accommodate busy professionals and individuals seeking treatment without disrupting their daily lives. We are proud to serve communities across Florida (Tampa Bay, St. Petersburg, Miami, Orlando, Boca Raton, West Palm Beach, Jacksonville, Fort Lauderdale, Naples, Sarasota).
- Programs are personalized for your sleep patterns, lifestyle, and goals. We don’t believe in one-size-fits-all solutions. Your initial assessment will involve a detailed discussion of your sleep history, daily routines, and any co-occurring mental health or medical conditions. We’ll often ask you to keep a sleep diary to gather objective data on your sleep patterns. This information allows us to tailor the CBT-I components—stimulus control, sleep restriction, cognitive therapy, and sleep hygiene—to your unique needs, ensuring the most effective and comfortable path to better sleep.
- Insurance accepted: Cigna, Optum, Florida Blue, and more. We strive to make evidence-based treatment accessible. We work with a wide range of insurance providers to help cover the cost of your CBT for insomnia program. You can verify your insurance in 2 minutes to see if you’re covered.
How Is CBT for Insomnia Delivered?
At Thrive Mental Health, we understand that access and convenience are crucial for consistent engagement and successful outcomes. That’s why we offer multiple delivery methods for CBT for insomnia:
- Individual therapy: This is the most common format, allowing for highly personalized treatment plans and one-on-one guidance from your therapist.
- Group therapy: For some, participating in a group setting can provide valuable support, shared learning, and a sense of community. Our Virtual Group Therapy Sessions offer a safe and engaging environment to work through sleep challenges together.
- Virtual options: We are pioneers in Telehealth for Mental Health, offering expert-led virtual programs that are just as effective as in-person sessions for many individuals. This dramatically increases accessibility, especially for those in remote areas or with mobility challenges. Digital CBT-I (dCBT-I) applications and online programs are also emerging tools that can supplement or precede therapist-led care.
- Evening and weekend sessions for busy professionals: We design our schedules to fit your life, not the other way around.
Finding a Qualified CBT for Insomnia Provider
Finding the right support is key. When seeking CBT for insomnia, look for licensed therapists, psychologists, or sleep specialists who have specific training and experience in this modality. Professional organizations like the Society of Behavioral Sleep Medicine and the American Board of Sleep Medicine can be excellent resources for finding qualified practitioners.
At Thrive Mental Health, our team is not only experienced and credentialed but also deeply committed to providing the highest standard of care. We pride ourselves on offering evidence-based treatments that are covered by major insurance plans, making transformative sleep therapy a reality for our clients.
FAQs: CBT for Insomnia—What People Ask (and What Actually Works)
How fast does CBT for insomnia work?
Most people notice better sleep in 2–4 sessions. Full results and sustained improvements are typically seen within 4–8 weeks (6-8 sessions), with effects lasting for up to 24 months or more post-treatment.
Can CBT for insomnia help if I have anxiety or depression?
Yes—absolutely! CBT for insomnia is highly effective even when you have co-occurring mental health conditions like anxiety or depression. In fact, improving sleep often leads to significant reductions in symptoms of these other disorders, demonstrating a powerful bidirectional benefit.
Is CBT for insomnia covered by insurance?
Yes—most major insurance plans, including Cigna, Optum, Florida Blue, and many others, provide coverage for CBT for insomnia. We encourage you to verify your specific benefits with us to understand your coverage.
Do I have to stop all sleep meds to start CBT for insomnia?
Not necessarily. While the long-term goal for many is to reduce or eliminate reliance on sleep medications, your Thrive therapist will work with you to create a safe, gradual, and individualized plan for medication management. The focus is on building sustainable sleep skills first.
Is virtual CBT for insomnia as effective as in-person?
Yes—research shows that virtual CBT for insomnia (dCBT-I) can be just as effective as face-to-face approaches for many people. It offers increased convenience and accessibility without compromising outcomes, making it a powerful tool for improving sleep.
Summary: Why CBT for Insomnia Is the Game-Changer You Need
If you’re tired of battling sleepless nights and the toll it takes on your life, CBT for insomnia is the fastest, safest, and most effective way to finally sleep through the night. Without pills, harmful side effects, or endless frustration, CBT-I empowers you with practical skills to rewire your brain for lasting rest. Our expert team at Thrive Mental Health delivers proven results, covered by insurance, with flexible virtual and in-person options across Florida. It’s time to stop dreading bedtime and start embracing restorative sleep.
Ready to Sleep Again? Take the First Step Now
Ready for support? Thrive offers virtual and hybrid IOP/PHP programs with evening options. Verify your insurance in 2 minutes (no obligation) → https://gothrivemh.com/verify-insurance or call 561-203-6085. If you’re in crisis, call/text 988.
Related: “How Virtual IOPs Cut Recovery Time by 50%” – Thrive Blog