From Chaos to Calm – Conditions Dialectical Behavior Therapy Can Help

When Emotions Feel Out of Control: What DBT Can Treat
Initial Disclaimer: If you are in a crisis or any other person may be in danger, please call or text 988 to reach the Suicide & Crisis Lifeline, or call 911 in the case of a medical emergency. You are not alone.
What is dialectical behavior therapy used to treat? DBT is proven to treat a wide range of mental health conditions, including:
- Borderline Personality Disorder (BPD) – the condition it was originally designed for
- Self-harm and suicidal behavior – reducing life-threatening actions
- Post-Traumatic Stress Disorder (PTSD) – managing trauma responses
- Substance use disorders – decreasing drug and alcohol use
- Eating disorders – addressing binge eating and bulimia
- Depression – especially treatment-resistant cases
- Anxiety disorders – managing intense worry and panic
- Bipolar disorder – stabilizing mood swings
If you’ve ever felt like your emotions hit harder, last longer, and spiral faster than other people’s—you’re not imagining it. Some brains are wired for emotional intensity. What might be a minor annoyance for someone else can feel like a tidal wave for you. A small rejection can trigger thoughts of worthlessness. A moment of stress can explode into rage or despair.
This isn’t a character flaw. It’s emotional dysregulation—and it’s treatable.
Dialectical Behavior Therapy (DBT) was built specifically for people who experience emotions this way. Originally developed by Dr. Marsha Linehan in the 1980s for individuals with chronic suicidal thoughts and borderline personality disorder, DBT has since become one of the most effective treatments for a range of conditions rooted in intense, difficult-to-manage emotions.
The results are measurable. Research shows DBT significantly reduces suicide attempts, psychiatric hospitalizations, emergency room visits, depression, anxiety, and substance use—while improving social functioning and quality of life. For people with borderline personality disorder, studies found that 77% no longer met diagnostic criteria after one year of DBT. Behavioral control—meaning the absence of suicidal or life-threatening behaviors—can often be achieved within just four to eight months.
What makes DBT different? It doesn’t just tell you to “think differently” or “calm down.” It teaches you practical skills to manage distress in the moment, regulate overwhelming emotions, steer relationships without burning bridges, and stay present instead of spiraling into the past or future. It balances acceptance (you’re doing the best you can) with change (you can learn to do better). And it works through a structured combination of individual therapy, group skills training, and real-time coaching when you need it most.
I’m Nate Raine, CEO of Thrive Mental Health, and I’ve spent over a decade building evidence-based behavioral health programs that integrate data, technology, and compassionate care. At Thrive, we specialize in helping individuals understand what is dialectical behavior therapy used to treat and delivering outcome-focused DBT programs to clients throughout Florida, meeting people where they are—whether that’s virtual, in-person, or a hybrid approach.
Basic what is dialectical behavior therapy used to treat glossary:
What is Dialectical Behavior Therapy (DBT) and How Does It Work?
Dialectical Behavior Therapy (DBT) is a highly effective, evidence-based psychotherapy (talk therapy) developed by Dr. Marsha Linehan. It’s rooted in Cognitive Behavioral Therapy (CBT) but was specifically adapted for individuals who experience emotions with extreme intensity and have difficulty regulating them. Imagine a therapy that acknowledges your pain while also empowering you with concrete tools to build a life worth living. That’s DBT.
At its heart, DBT operates on a “dialectical” philosophy, which means finding a balance between two seemingly opposing ideas: acceptance and change. We help you learn to accept your current reality, emotions, and thoughts without judgment, while simultaneously working towards making positive changes to replace unhelpful behaviors with more effective ones. This balance is crucial for healing, enabling you to move forward rather than getting stuck in self-blame or resistance.
DBT’s approach is also informed by the biosocial theory, which posits that emotional dysregulation often stems from a biological predisposition to high emotional sensitivity and reactivity interacting with an invalidating environment. This leads to a struggle with understanding, labeling, and regulating intense emotions, often resulting in impulsive or self-destructive behaviors. DBT addresses this by providing structured tools and a validating environment.
For a deeper dive into how our programs integrate these principles, explore More info about DBT treatments.
The Core DBT Skills That Build a Life Worth Living
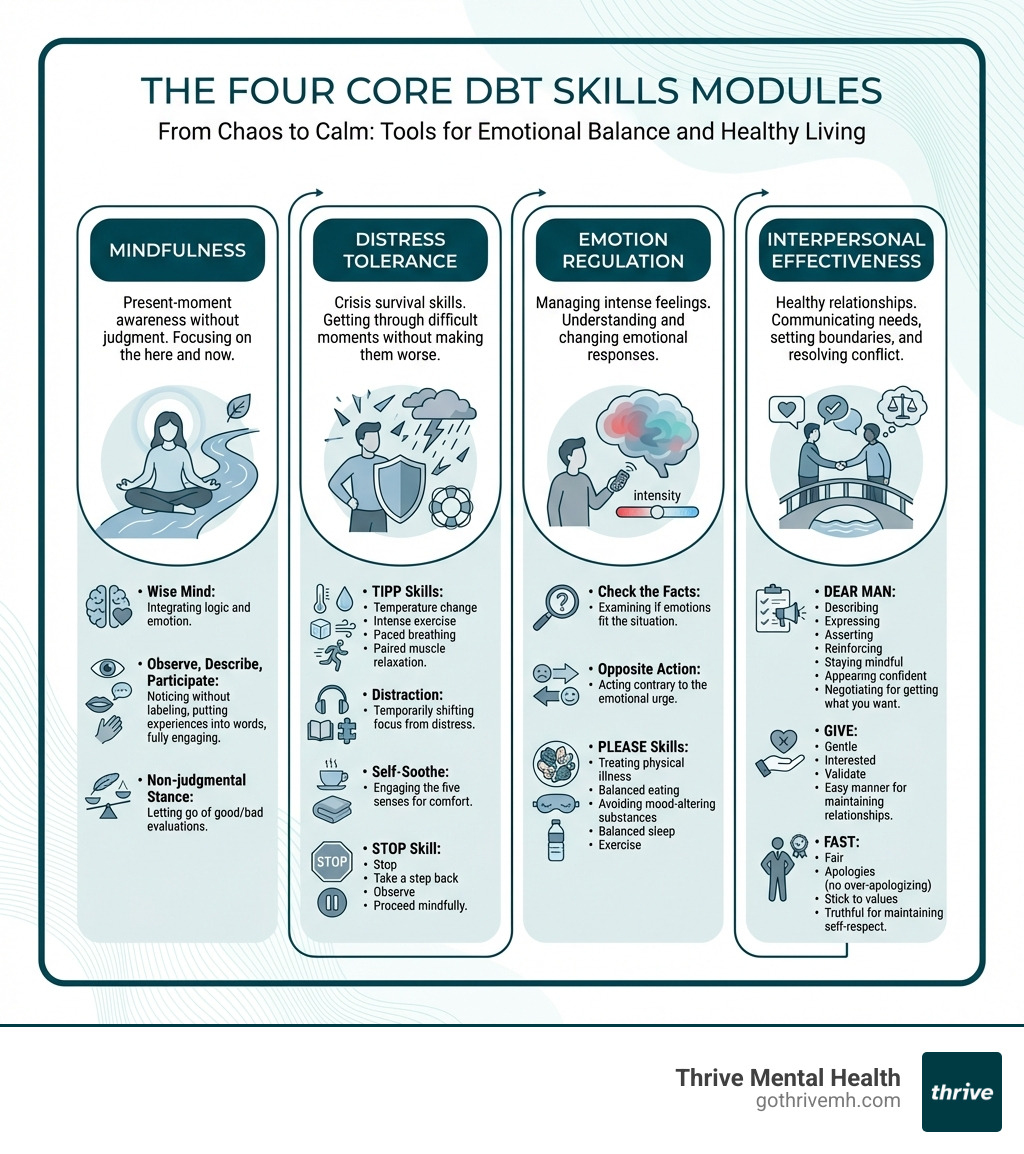
The power of DBT lies in its practical, teachable skills. These aren’t just abstract concepts; they are concrete techniques you can use in your daily life to steer difficult situations and intense emotions. We focus on four core modules:
- Mindfulness: This is the foundation of all DBT skills. Mindfulness teaches you to pay attention to the present moment without judgment. It helps you observe your thoughts, feelings, and sensations as they are, rather than getting swept away by them. By practicing mindfulness, you can gain a sense of control over your attention and become more aware of your experiences, leading to a calmer, more focused existence.
- Distress Tolerance: Life throws curveballs, and sometimes, you simply can’t change a painful situation immediately. Distress tolerance skills teach you how to get through a crisis without making things worse. These skills include self-soothing, distraction, improving the moment, and radical acceptance. Radical acceptance involves accepting reality as it is, even if it’s painful, which can reduce suffering and help you move towards problem-solving.
- Emotion Regulation: For individuals struggling with intense emotions, this module is a game-changer. Emotion regulation skills help you understand, identify, and manage your emotions more effectively. You learn to reduce your emotional vulnerability, change unwanted emotions, and increase positive emotional experiences. This means feeling less overwhelmed, less reactive, and more in control of your emotional life.
- Interpersonal Effectiveness: Relationships are often a source of both joy and pain. These skills focus on how to ask for what you need, say no, and steer conflict while maintaining self-respect and strengthening your relationships. You learn to communicate assertively, listen effectively, and build healthy boundaries, leading to more stable and fulfilling connections.
These skills are taught and practiced, with the ultimate goal of helping you build a “life worth living.” Our commitment to evidence-based practices is strong, as demonstrated by the Scientific research on DBT’s effectiveness.
How DBT Is Different From Traditional CBT
While DBT grew out of Cognitive Behavioral Therapy (CBT), it has distinct features that make it uniquely effective for emotional dysregulation. Here’s a quick look at how they compare:
| Feature | Traditional CBT | Dialectical Behavior Therapy (DBT) |
|---|---|---|
| Core Principle | Primarily focuses on changing dysfunctional thoughts and behaviors. | Balances acceptance of current reality with the need for change (the “dialectical” aspect). |
| Emotional Intensity | Often assumes negative thoughts are distortions to be “swapped” or challenged. | Acknowledges that intense emotions and thoughts often make sense given an individual’s experiences; emphasizes validation. |
| Validation | May not explicitly prioritize validating feelings before addressing change. | Heavily emphasizes validation—acknowledging the validity of a person’s experience, even if you don’t agree with their behavior. |
| Mindfulness | May be incorporated, but not a central, foundational skill. | A core, foundational skill taught explicitly and integrated throughout all modules. |
| Therapist Role | Often more directive in challenging thoughts. | Balances acceptance and change, acts as a coach, and maintains a non-judgmental stance. |
| Target Population | Broad range of mental health conditions. | Specifically designed for individuals with severe emotional dysregulation, often with suicidal ideation, self-harm, and BPD. |
| Relationship Focus | May address relationships, but not as as DBT. | Strong emphasis on interpersonal effectiveness skills to build and maintain healthy relationships. |
| Crisis Intervention | Focus on coping strategies. | Includes phone coaching for in-the-moment crisis intervention and skill application. |
DBT’s unique emphasis on validation and its dialectical approach allows us to meet you where you are, acknowledging your struggles, before guiding you toward effective change. This nuanced approach is why it’s so powerful for individuals who haven’t found success with other therapies. Learn more about their distinctions on our blog: DBT vs. CBT differences.
What is Dialectical Behavior Therapy Used to Treat? [Full List]
At Thrive Mental Health, we see firsthand across Florida how what is dialectical behavior therapy used to treat extends far beyond its original scope, offering hope and healing to many who struggle with intense emotional dysregulation, self-destructive behaviors, and interpersonal difficulties. Its proven effectiveness in reducing psychiatric hospitalizations, emergency room visits, and improving social functioning makes it a cornerstone of our treatment philosophy.

Borderline Personality Disorder (BPD): The Original Focus of DBT
Callout Box: If you’re struggling with thoughts of self-harm or suicide, call or text 988 now. Help is available 24/7.
DBT was initially developed by Dr. Marsha Linehan specifically for chronically suicidal individuals, many of whom met the criteria for Borderline Personality Disorder (BPD). This complex condition is characterized by a pervasive pattern of instability in relationships, self-image, emotions, and impulsivity. Individuals with BPD often experience:
- Chronic suicidal ideation and behaviors: A persistent preoccupation with death or suicide, and parasuicidal behaviors (self-harm without lethal intent, such as cutting or burning). For parasuicidal BPD patients, DBT consistently leads to superior reductions in these life-threatening behaviors compared to other treatments.
- Intense fear of abandonment: Often leading to frantic efforts to avoid real or imagined rejection.
- Unstable and chaotic relationships: Characterized by rapid shifts between idealization and devaluation.
- Impulsivity: Engaging in risky behaviors like substance abuse, reckless driving, or binge eating.
- Severe mood swings: Rapid and intense shifts in emotional states.
The statistics on DBT’s impact on BPD are compelling. Studies show that DBT patients experience greater reductions in suicide attempts, psychiatric hospitalization, angry behavior, and emergency room visits. Furthermore, a significant 77% of DBT patients no longer met the criteria for a BPD diagnosis after just one year of treatment. This profound impact underscores why DBT is considered the most effective treatment for BPD. Dive deeper into how DBT can transform lives on our blog: More info on how DBT improves mental health.
What is dialectical behavior therapy used to treat beyond BPD?
While BPD remains a primary focus, the skills taught in DBT are universally beneficial for anyone struggling with emotional dysregulation. We’ve seen its effectiveness across a spectrum of other mental health conditions, including:
- Post-Traumatic Stress Disorder (PTSD): DBT helps individuals with PTSD manage intense emotional responses to trauma, reduce impulsive behaviors, and improve their ability to tolerate distress. It provides a structured approach to process difficult emotions and regain control.
- Substance Use Disorders (SUDs): For individuals battling addiction, especially those with co-occurring BPD, DBT has shown remarkable success. Patients undergoing DBT experienced greater reductions in drug use during treatment and follow-up periods, along with lower dropout rates, compared to control groups. This is because DBT equips individuals with coping skills to manage cravings and emotional triggers without resorting to substances.
- Eating Disorders (Binge Eating, Bulimia): DBT has demonstrated significant improvements for individuals with eating disorders like binge eating disorder and bulimia. Patients showed greater improvements in bingeing episodes, body image concerns, eating concerns, and anger. One study found that 86% of participants stopped bingeing by the end of treatment.
- Treatment-Resistant Depression: When traditional antidepressant medications and therapies haven’t yielded sufficient results, DBT can offer a new path forward. For depressed elderly patients with personality disorders, a larger proportion of DBT patients achieved remission from depression post-treatment and at follow-up compared to medication-only treatment. DBT helps individuals manage the intense negative emotions often underlying persistent depression.
- Bipolar Disorder: DBT can assist individuals with bipolar disorder in stabilizing mood swings and reducing impulsive behaviors often associated with manic or depressive episodes. The emotion regulation and distress tolerance skills are particularly valuable in managing the extreme highs and lows.
- Anxiety Disorders: For those who experience intense anxiety, panic attacks, or generalized worry, DBT provides powerful tools to manage distressing thoughts and physical sensations. Mindfulness helps in observing anxiety without judgment, while distress tolerance skills enable individuals to ride out anxious moments without escalating them.
- Attention Deficit Hyperactivity Disorder (ADHD): While not a primary treatment for ADHD, some adaptations of DBT have shown promise in helping individuals with ADHD manage emotional dysregulation, impulsivity, and improve executive functioning skills that are often impacted by intense emotions.
What to Expect from a DBT Program [Commitment & Structure]
A comprehensive DBT program is structured and intensive, designed to provide maximum support and skill-building. It’s not just a weekly therapy session; it’s a holistic approach that integrates several components to ensure you’re equipped to handle life’s challenges. Typically, a full DBT program includes:

- Individual Therapy: You’ll have weekly one-on-one sessions with a DBT therapist, usually lasting 45-60 minutes. These sessions are highly focused, addressing your specific goals and behaviors that interfere with your progress or quality of life. The therapist helps you apply the skills learned in group to your personal situations. We use “diary cards” as homework to track emotions and actions, helping you identify patterns and triggers, which then informs our collaborative work in sessions.
- Group Skills Training: This is where you learn the core DBT skills (Mindfulness, Distress Tolerance, Emotion Regulation, Interpersonal Effectiveness) in a supportive group setting. Group sessions typically run for 1.5-2.5 hours weekly, often lasting 6 to 12 months to cover all modules. It’s a fantastic environment for practicing new behaviors and receiving feedback from peers and therapists.
- Phone Coaching: Imagine having access to your therapist for in-the-moment guidance when you’re facing a crisis or struggling to apply a skill. Phone coaching is an essential component of DBT, providing real-time support to prevent self-destructive behaviors and help you generalize skills into your daily life. It’s not about being available 24/7, but about teaching you effective help-seeking and skill application during critical moments.
- Therapist Consultation Team: This is a weekly meeting where DBT therapists collaborate to support each other, ensure adherence to the DBT model, and troubleshoot challenging cases. This component helps maintain therapist motivation and competence, which is crucial for delivering effective treatment.
The commitment required for a comprehensive DBT program is significant, typically lasting 6 to 12 months, and sometimes longer for more complex cases. However, the intensity pays off. Behavioral control—meaning the absence of suicidal or other life-threatening behaviors—can often be achieved within just four to eight months. For adults and young professionals across Florida, our virtual and hybrid Intensive Outpatient (IOP) and Partial Hospitalization (PHP) programs integrate these DBT components, offering flexible scheduling and measurable results. Learn more about our approach to online DBT: More info about virtual DBT IOP.
How to Find a Qualified DBT Therapist
Finding the right therapist is a critical step. When looking for someone to help you understand what is dialectical behavior therapy used to treat and guide you through the process, find a qualified professional. We recommend the following:
- Seek Licensed Professionals: Always ensure your therapist is state-certified and licensed. In Florida, this means a psychologist, psychiatrist, Licensed Clinical Social Worker (LCSW), Licensed Marriage and Family Therapist (LMFT), or Licensed Professional Counselor (LPC).
- Look for Specialized DBT Training: DBT is a specialized modality. Ask potential therapists about their training in DBT. Ideally, they should have completed a specialized DBT training or certificate program. Organizations like Behavioral Tech, LLC (founded by Dr. Marsha Linehan) offer such training.
- Ask Key Questions: Don’t hesitate to interview potential therapists. Important questions include:
- “Do you provide comprehensive DBT, including individual therapy, group skills training, phone coaching, and a consultation team? Or do you offer a modification, and why?”
- “Are you part of a DBT consultation team, and who are its members?”
- “What is your policy regarding phone calls or emails between sessions?”
- “What is the expected initial commitment for therapy?”
- Consider Program Levels: For those needing more intensive support than weekly outpatient sessions, look for programs like our Intensive Outpatient (IOP) or Partial Hospitalization (PHP) programs, which often integrate comprehensive DBT. These programs are designed for people who need more than once-a-week therapy but less than inpatient care.
- Verify Insurance Coverage: Financial accessibility is important. Many insurance providers, including Aetna, Cigna, Optum, and Florida Blue, may cover DBT treatment. We encourage you to verify your benefits to understand your coverage options.
Frequently Asked Questions about DBT
What is the main goal of DBT?
The main goal of DBT is to help people build a “life worth living” by teaching skills to manage intense emotions, reduce self-destructive behaviors, and improve relationships, balancing acceptance of who you are with the need for change. It empowers you to move from a state of emotional chaos to one of stability and fulfillment.
How long does it take for DBT to work?
While some skills offer immediate relief, comprehensive DBT is a long-term commitment, typically lasting 6 to 12 months to achieve lasting behavioral change. Studies show significant reductions in life-threatening behaviors can often be achieved within four to eight months. The journey is an investment in yourself, with profound and enduring rewards.
Can you do DBT on your own?
While self-help workbooks and apps exist, standard DBT is most effective when delivered by a trained therapist through a structured program including individual therapy, group skills training, and phone coaching. This provides the necessary support, accountability, and expert guidance to truly master these complex skills and apply them effectively in your life.
Take the First Step Towards Calm with Thrive Mental Health
Understanding what is dialectical behavior therapy used to treat is the first step towards a more stable, fulfilling life. At Thrive Mental Health, we are dedicated to providing evidence-based treatment for emotional dysregulation and related conditions. Our virtual and in-person Intensive Outpatient (IOP) and Partial Hospitalization (PHP) programs in Florida are designed specifically for adults and young professionals who need comprehensive support. With flexible scheduling and a focus on measurable results, our expert-led care can help you move from chaos to calm.
Ready for support in Florida? Thrive offers virtual and hybrid IOP/PHP programs with evening options. Verify your insurance in 2 minutes (no obligation) or call 561-203-6085. If you’re in crisis, call/text 988.