Trauma Recovery: Finding Your Path to Healing Through Therapy

Why Therapy for Trauma Recovery Changes Everything
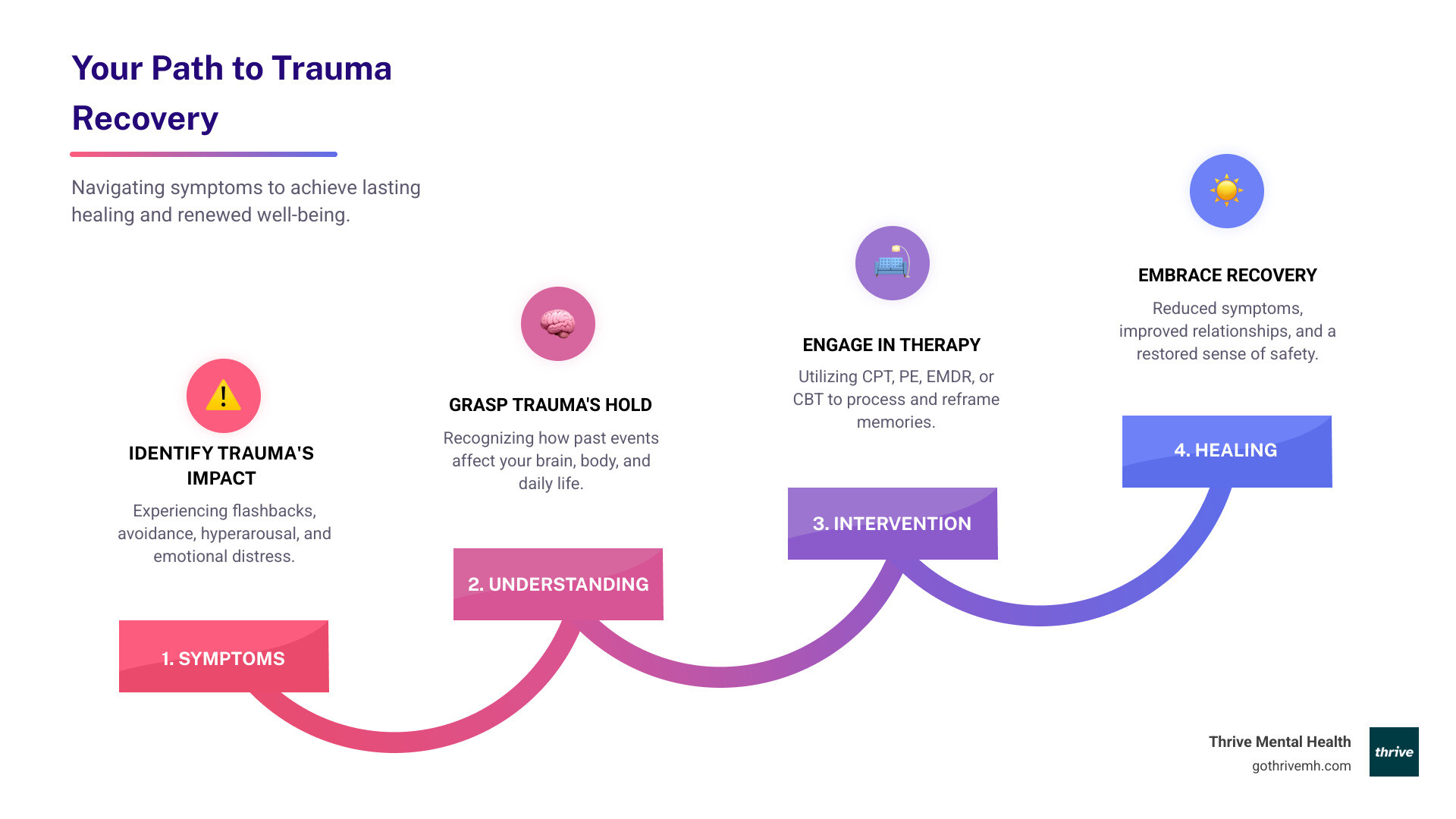
Therapy for trauma recovery helps you move from feeling controlled by the past to living fully in the present. If you’ve experienced a traumatic event—whether it was a car accident, assault, childhood abuse, or the sudden loss of someone close—you know how deeply it can affect your daily life, relationships, and sense of safety.
Quick Answer: What Works for Trauma Recovery?
The most effective, evidence-based therapies for trauma include:
- Cognitive Processing Therapy (CPT) – Challenges unhelpful beliefs about the trauma (typically 12 sessions)
- Prolonged Exposure (PE) – Gradually confronts trauma memories and avoided situations (12-16 sessions over 3 months)
- Eye Movement Desensitization and Reprocessing (EMDR) – Reprocesses traumatic memories using bilateral stimulation (6-12 sessions)
- Cognitive Behavioral Therapy (CBT) – Targets the relationship between thoughts, feelings, and behaviors (12-16 sessions)
All are strongly recommended by the American Psychological Association for treating PTSD.
Trauma is more common than you might think. Over 70% of people experience a traumatic event at least once in their lifetime, and approximately 10% develop posttraumatic stress disorder (PTSD) as a result. The good news? Research shows that structured, trauma-focused therapy works—and it can work faster than you expect.
This guide walks you through the evidence-based therapy options for trauma recovery, what to expect from treatment, and how to find the right level of care for your needs—whether that’s weekly therapy, virtual sessions, or a more intensive program.
I’m Nate Raine, CEO of Thrive Mental Health, and I’ve spent over a decade leading behavioral health and digital change initiatives that integrate evidence-based clinical care with measurable outcomes. At Thrive, we specialize in delivering personalized therapy for trauma recovery through our virtual and hybrid IOP/PHP programs, designed for adults and young professionals in Florida ready to reclaim their lives.
Therapy for trauma recovery word roundup:
- Somatic Therapy vs. EMDR: Which is Right For You?
- benefits of emdr therapy
- Why Do I Feel Like a Burden? — and How to Heal
If you are in crisis or considering self-harm, please call or text 988 to reach the Suicide & Crisis Lifeline. You are not alone, and help is available 24/7.
Understanding Trauma’s Grip: Why You Feel the Way You Do
Trauma can leave a profound and often confusing impact on our lives. It’s not just about what happened, but how our minds and bodies reacted and continue to react to it. Understanding this impact is the first step toward effective therapy for trauma recovery.
What is Trauma and How Does It Affect You?
Tra4uma is formally defined as exposure to death, severe injury, or sexual violence, which can occur directly to an individual, through witnessing the event, indirectly, or via repeated exposure to distressing details. The Substance Abuse and Mental Health Services Administration (SAMHSA) further defines individual trauma as an event, series of events, or set of circumstances experienced as physically and emotionally harmful or life-threatening, with lasting adverse effects on functioning and well-being.
What’s crucial to understand is that trauma is highly subjective. The same event can be significantly more traumatic for some individuals than for others. This isn’t a sign of weakness; it’s a reflection of our unique biology, past experiences, and support systems.
The effects of trauma are not just emotional or psychological; they are deeply physiological. Traumatic incidents can distort our emotions, memory, consciousness, and self-perception, affecting our interpersonal connections, attachment patterns, and overall brain and body function. Our bodies, in an attempt to protect us, can get stuck in a “fight, flight, or freeze” response, leading to chronic emotional dysregulation, anxiety, and even physical symptoms. This is why specialized therapy for trauma recovery is so vital.

Signs You Might Be Struggling with Unresolved Trauma or PTSD
When the thoughts and memories of a traumatic event don’t fade or even worsen over time, they can lead to posttraumatic stress disorder (PTSD). PTSD can seriously disrupt a person’s ability to regulate their emotions and maintain healthy relationships. Recognizing the signs is key to seeking help. Common symptoms include:
- Re-experiencing: This involves intrusive thoughts, flashbacks where you feel like you’re reliving the event, and distressing nightmares. These are the brain’s way of trying to process the unprocessed memory, often leading to intense emotional and physical reactions.
- Avoidance: You might find yourself actively avoiding people, places, activities, objects, or even thoughts and feelings that remind you of the traumatic event. This avoidance can become so pervasive that it significantly limits your life.
- Hyperarousal: This category includes symptoms like hypervigilance (being constantly on guard), irritability, difficulty sleeping, and being easily startled. Your nervous system is essentially stuck in overdrive, perceiving threats even when none are present.
- Negative changes in mood and cognition: You might experience persistent negative beliefs about yourself, others, or the world, such as intense guilt or shame. Memory loss related to the trauma, a sense of detachment from others, and a diminished interest in activities you once enjoyed are also common.
These symptoms aren’t just “in your head”; they are real, measurable impacts of trauma on your brain and body.
Simple vs. Complex PTSD: Why the Distinction Matters
While all trauma is distressing, understanding the different types can help tailor therapy for trauma recovery.
- Simple PTSD: This typically arises from a single, isolated traumatic event. Examples include a car accident, a violent assault, or a natural disaster. While deeply impactful, the trauma has a clear beginning and end.
- Complex PTSD (C-PTSD): This often develops from prolonged, repeated, and inescapable traumatic experiences, particularly those occurring in childhood or within relationships where the victim is dependent on the perpetrator. Examples include ongoing childhood neglect, sexual or physical abuse, domestic violence, or prolonged captivity.
The key difference lies in the pervasive nature of C-PTSD. Because it often occurs during critical developmental periods, it can profoundly affect a person’s ability to regulate their emotions, form healthy attachments, and maintain stable relationships. Individuals with C-PTSD may struggle with their sense of self, experience chronic dissociation, and have difficulty trusting others. Effective therapy for trauma recovery for C-PTSD, like the programs we offer in Florida, often requires a more phased and integrative approach.
Evidence-Based Therapy for Trauma Recovery: Treatments That Work
When it comes to healing from trauma, we don’t believe in guesswork. Our approach at Thrive Mental Health is grounded in evidence-based treatments—the gold standard for addressing PTSD and other trauma-related conditions. These are the therapies that have been rigorously studied and proven to be effective.
The American Psychological Association (APA) provides comprehensive clinical practice guidelines for the treatment of PTSD, distinguishing between strongly recommended and conditionally recommended interventions. We align our programs with these guidelines, ensuring you receive the most effective care. You can review the full APA Clinical Practice Guideline for PTSD for more detailed information.
To give you a clear overview, here’s a comparison of some key trauma therapies:
– – – – – – – – – – – – — – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – – –
| Cognitive Processing Therapy (CPT) | Challenges un-helpful beliefs about the trauma | T-ypically 1-2 sessions | Focuses on how thoughts about the trauma affect current feelings. |
| Prolonged Exposure (PE) | Gradually confronts trauma memories and avoided situations | 12-1-6 sessions over 3 months | Repeated exposure to trauma memories (imaginal) and safe avoided situations (in-vivo). |
| Eye Movement Desensitization and Reprocessing (EMDR) | Reprocesses traumatic memories using bilateral stimulation | 6-12 sessions (60-90 min each) | Uses guided eye movements or other bilateral stimulation to help the brain process distressing memories. |
| Cognitive Behavioral Therapy (CBT) | Targets the relationship between thoughts, feelings, and behaviors | 12-16 sessions | Identifies and changes unhelpful thinking patterns and behaviors related to trauma. |
| Narrative Exposure Therapy (NET) | Establishes a coherent life story by creating a chronological narrative of experiences | Varies | Helps contextualize traumatic events within a life journey, reducing fragmentation. |
| Psychodynamic Therapy | Explores unconscious conflicts and early life experiences | V-aries | Understands how past relationships influence present reactions to trauma. |
| Sensorimotor Psychotherapy | Focuses on the body’s experience of trauma | Varies | Processes traumatic memories by observing and integrating physical sensations and movements. |
Cognitive Therapies: Rewiring Your Thoughts About Trauma
Cognitive therapies are a cornerstone of therapy for trauma recovery, focusing on how our thoughts, feelings, and behaviors are interconnected. By addressing maladaptive thought patterns, these therapies help us regain control over our emotional responses.
- Cognitive Behavioral Therapy (CBT): This broad approach focuses on the relationships among thoughts, feelings, and behaviors, targeting current problems and symptoms. For trauma, CBT helps you identify and change negative thinking patterns that maintain your distress.
- Cognitive Processing Therapy (CPT): A specific type of CBT, CPT helps you modify and challenge unhelpful beliefs—what we call \”stuck points\”—related to the trauma. It addresses questions like \”Why did this happen?\” or \”What does this say about me?\” This approach helps you develop more balanced and helpful ways of thinking about the traumatic event and its aftermath. CPT is typically delivered over 12 sessions.
- Prolonged Exposure (PE): PE is another powerful CBT-based therapy that teaches you to gradually approach trauma-related memories, feelings, and situations that you’ve been avoiding. This is done through two main components:
- Imaginal exposure: Repeatedly recounting the traumatic memory in detail, which helps reduce its emotional intensity.
- In-vivo exposure: Gradually confronting safe but avoided situations, places, or objects in real life.
PE is typically provided over a period of about three months with weekly individual sessions, often needing 60- to 120-minute sessions.
The effectiveness of these cognitive therapies is well-documented. For instance, studies show CPT leads to a significant reduction in PTSD symptoms, with a standardized mean difference (SMD) of 1.40 lower compared to controls, and PE therapy boasts an SMD of 1.27 lower for PTSD symptom reduction. These are not just incremental changes; they represent profound healing.
How EMDR Therapy Helps Your Brain Reprocess and Heal
Eye Movement Desensitization and Reprocessing (EMDR) therapy is a unique and highly effective mental health treatment technique that has transformed therapy for trauma recovery. It involves moving your eyes in a specific way while processing traumatic memories, allowing your brain to heal itself.
EMDR therapy relies on the Adaptive Information Processing (AIP) model, which posits that traumatic memories can become \”stuck\” or improperly stored in the brain, leading to symptoms like flashbacks and intrusive thoughts. EMDR helps to \”unstick\” these memories. During an EMDR session, you focus on a distressing memory while simultaneously engaging in bilateral stimulation (e.g., guided eye movements, tapping, or auditory tones). This process helps your brain reprocess the memory, changing it into something less heavy and invasive, allowing it to be experienced more calmly and less painfully.
EMDR can help with a wide range of trauma, not just PTSD. While most widely used for PTSD, it also treats anxiety disorders, depression disorders, dissociative disorders, eating disorders, obsessive-compulsive disorders, personality disorders, and acute stress disorder. Research even explores EMDR beyond PTSD, showing its versatility.
A typical EMDR therapy course consists of 6 to 12 sessions, each lasting approximately 60 to 90 minutes. Many clients experience significant improvement in under ten sessions, finding relief from distressing symptoms and a renewed sense of peace.
Other Powerful Approaches to Therapy for Trauma Recovery
While CBT, CPT, PE, and EMDR are frontline treatments, other modalities offer valuable pathways in therapy for trauma recovery:
- Narrative Exposure Therapy (NET): This approach helps individuals, particularly those who have experienced multiple or prolonged traumas, to establish a coherent life story. By creating a chronological narrative of their experiences, individuals can contextualize traumatic events within their life’s journey, reducing fragmentation and promoting integration.
- Psychodynamic Therapy: This form of therapy explores unconscious conflicts and early life experiences that may contribute to current trauma responses. It helps individuals understand how past relationships and unresolved issues influence their present reactions to trauma.
- Sensorimotor Psychotherapy: Recognizing that trauma is stored not just in the mind but also in the body, sensorimotor psychotherapy focuses on the body’s experience of trauma. It helps individuals process traumatic memories by observing and integrating physical sensations, movements, and postures, leading to a deeper release of stored trauma.
At Thrive Mental Health, we believe in a holistic approach. Our Florida-based programs offer various specialized modalities to meet diverse needs. You can learn more about our comprehensive treatment modalities and how they can support your healing journey.
Your Healing Journey: What to Expect from Start to Finish
Starting on therapy for trauma recovery is a courageous step. It’s natural to wonder what the process will entail. We believe in transparency and empowering you with knowledge about what to expect, from your first session to long-term healing.

The 3 Phases of Trauma Recovery You’ll Move Through
Trauma recovery isn’t a linear path, but it often follows a phased framework, as conceived by Dr. Pierre Janet in the late 1800s and popularized by Dr. Judith Herman. This structured approach helps ensure a safe and effective healing process:
- Phase 1: Safety and Stabilization: This is the crucial first step. Before delving into traumatic memories, we focus on establishing a sense of safety in your current life and equipping you with coping skills. This includes learning emotional regulation techniques, managing acute distress, and building a stable support system. Regaining a sense of safety may take days to weeks for acutely traumatized individuals or months to years for those who have experienced ongoing or chronic abuse.
- Phase 2: Remembrance and Mourning: Once you feel stable and have robust coping mechanisms, therapy shifts to processing the trauma itself. This involves carefully revisiting and working through traumatic memories, putting words and emotions to them, and making meaning of your experiences. This phase also provides space to mourn the losses associated with the trauma—losses of safety, innocence, relationships, or future expectations. The pacing and timing here are crucial to prevent re-traumatization.
- Phase 3: Reconnection and Integration: The final phase focuses on moving forward. It involves creating a new sense of self and future, redefining yourself not by your trauma, but by your resilience and growth. You’ll work on integrating your traumatic experiences into your life story in a way that doesn’t define you but rather informs who you’ve become. This phase emphasizes building meaningful relationships, finding purpose, and living a fulfilling life.
What Happens During a Trauma Therapy Session?
While every individual’s journey is unique, a typical course of therapy for trauma recovery generally follows a predictable structure:
- Initial Assessment: Your therapist will conduct a thorough assessment to understand your history, the nature of your traumatic experiences, your current symptoms, and your goals for therapy. This helps us tailor a treatment plan specifically for you.
- Building Rapport: A safe, trusting relationship with your therapist is paramount in trauma work. We prioritize creating an environment where you feel heard, validated, and secure enough to explore difficult emotions.
- In-Session Work: Depending on the therapeutic modality chosen (CBT, CPT, PE, EMDR, etc.), sessions will involve specific techniques. This could range from challenging negative thought patterns, practicing exposure exercises, engaging in bilateral stimulation, or developing new coping strategies.
- Psychoeducation: A vital component of trauma therapy is understanding how trauma affects the brain and body. Your therapist will provide psychoeducation, helping you normalize your reactions and empowering you with knowledge about your healing process.
How Long Does Therapy for Trauma Recovery Take?
One of the most common questions we hear is, “How long will this take?” The duration of therapy for trauma recovery varies significantly based on individual needs, the type and severity of the trauma, and the chosen therapeutic approach.
For single-incident trauma, many effective therapies can be relatively short-term:
- EMDR therapy often sees significant progress between 6 and 12 sessions.
- CPT is typically delivered over 12 sessions.
- CBT is often completed within 12-16 sessions.
However, for individuals with complex trauma (C-PTSD) resulting from chronic, prolonged experiences, the healing journey may require more extended support, potentially lasting a year or more. The most important thing is to focus on progress and not a fixed timeline. Our goal at Thrive Mental Health is to equip you with lasting tools and resilience, not just a quick fix. Our Florida-based IOP and PHP programs are designed to provide this extended support when needed.
Finding the Right Help: Therapists, Programs, and Insurance
Taking the first step towards therapy for trauma recovery means making informed choices. It’s about finding the right fit for your unique needs, whether that involves a specific therapist, a particular program structure, or understanding how your insurance can support your healing.
What is Trauma-Informed Care (and Why It’s Non-Negotiable)?
Trauma-informed care (TIC) represents a fundamental shift in how we approach mental health. It moves away from the question, “What’s wrong with you?” to a more compassionate and empowering inquiry: “What happened to you?” This paradigm shift, first introduced in 2001 by Harris and Fallot, recognizes the widespread impact of trauma and integrates this understanding into all aspects of service delivery.
The key principles of trauma-informed care include:
- Safety: Ensuring physical and emotional safety for clients and staff.
- Trustworthiness and Transparency: Building trust through clear communication and consistent boundaries.
- Peer Support: Utilizing individuals with lived experience to foster hope and connection.
- Collaboration and Mutuality: Sharing power and decision-making between clients and providers.
- Empowerment, Voice, and Choice: Valuing and strengthening clients’ voices and self-advocacy.
- Cultural, Historical, and Gender Considerations: Recognizing and addressing cultural biases and historical trauma.
At Thrive Mental Health, we embed these principles into every aspect of our programs. We understand that public institutions and service systems can sometimes be trauma-inducing. Therefore, we are committed to actively resisting re-traumatization in our treatment settings, ensuring a truly safe and healing environment. This commitment to TIC is supported by robust research on trauma-informed care principles.
How to Find a Qualified Trauma Therapist in Florida or Online
Finding the right professional for therapy for trauma recovery is a critical decision. Here’s what we recommend:
- Look for Specific Credentials and Certifications: Seek out licensed professionals such as Licensed Clinical Social Workers (LCSW), Psychologists (PhD or PsyD), or Licensed Professional Counselors (LPC) who have specialized training. Crucially, look for certifications in specific trauma modalities like EMDR, CPT, or PE.
- Ask the Right Questions: When you connect with a potential therapist, don’t hesitate to ask about their experience with your specific type of trauma, their therapeutic approach, and how they implement trauma-informed care. A good therapist will welcome these questions.
- Consider Virtual vs. In-Person: With the rise of telehealth, you have more options than ever. Virtual therapy offers flexibility and accessibility, which can be particularly beneficial for those in Florida, where Thrive Mental Health offers specialized virtual IOPs. For some, in-person sessions offer a preferred level of connection.
- Use Your Insurance: Navigating insurance can feel daunting, but it’s a vital step to making therapy accessible. Many plans, including Cigna, Optum, and Florida Blue, offer coverage for mental health services. We encourage you to check your benefits. You can easily verify your insurance coverage with us in minutes to understand your options.
When You Need More Than Weekly Sessions: IOP & PHP Programs
For many individuals, weekly therapy sessions are sufficient. However, if you’re struggling with severe trauma symptoms, have co-occurring mental health challenges, or find that weekly sessions aren’t providing enough support, a more intensive program might be what you need.
Thrive Mental Health specializes in providing structured, evidence-based care through our Intensive Outpatient (IOP) and Partial Hospitalization (PHP) programs, available virtually and in-person across Florida. These programs are designed for adults and young professionals who need more than once-a-week therapy but less than inpatient care.
- Intensive Outpatient Programs (IOP): Our IOPs offer several hours of therapy, several days a week, providing a higher level of support and structure while allowing you to live at home and manage other responsibilities. This format allows for accelerated progress and deeper engagement with therapy for trauma recovery. Learn about our Virtual IOP options.
- Partial Hospitalization Programs (PHP): PHPs provide an even more intensive level of care, typically involving a full day of programming, five days a week. This is ideal for those requiring significant support and stabilization, offering a therapeutic environment similar to inpatient care but without overnight stays. Explore our PHP programs.
The benefits of these intensive programs include accelerated progress, highly structured support, and a built-in community of peers, all contributing to a more robust and sustainable healing journey.
Frequently Asked Questions about Therapy for Trauma
We understand you have questions, and we’re here to provide clear, concise answers to some of the most common inquiries about therapy for trauma recovery.
Can trauma ever be fully “cured”?
The concept of “curing” trauma is complex. While the memory of a traumatic event will always exist, the goal of therapy for trauma recovery is not to erase it, but to transform its impact. Recovery means the past no longer controls your present. Your symptoms can be managed to the point where they no longer disrupt your daily life, relationships, and emotional well-being. We aim for integration, where the trauma becomes a part of your life story, but not the defining chapter. You can absolutely reclaim your life and find peace.
What is the most effective therapy for PTSD?
According to the American Psychological Association (APA) guidelines, several trauma-focused psychotherapies are strongly recommended due to their robust evidence base. These include Cognitive Processing Therapy (CPT), Prolonged Exposure (PE), and Cognitive Behavioral Therapy (CBT). Eye Movement Desensitization and Reprocessing (EMDR) is also highly effective and widely recognized. The “best” therapy for you will depend on your individual needs, the nature of your trauma, and your personal preferences, as well as the expertise of your therapist. Often, a combination of approaches or finding the right therapist-client fit is key.
Will talking about my trauma in therapy make it worse?
It’s a very common and valid concern to worry that discussing your trauma will re-traumatize you or make things worse. While it’s true that engaging with traumatic memories in therapy can be difficult and bring up intense emotions, a skilled trauma therapist is trained to guide this process safely. They will first help you build coping skills and establish a sense of safety and stability. The process is gradual, controlled, and aims to reduce the emotional charge of the memory over time, rather than simply reliving the pain. We work at your pace, ensuring you feel supported and empowered throughout.
Take the First Step Toward Reclaiming Your Life
Healing from trauma is a journey, not a destination. But with evidence-based therapy for trauma recovery, a clear path forward exists. You don’t have to carry the weight of the past alone. We believe you have the power to choose your path to recovery and reclaim a life filled with purpose, connection, and peace.
Thrive Mental Health offers flexible, expert-led virtual and in-person IOP/PHP programs in Florida, designed for adults and young professionals who are ready for real change. Our programs integrate clinical expertise with measurable results, making effective therapy for trauma recovery accessible throughout the state.
Ready for support? Thrive offers virtual and hybrid IOP/PHP programs with evening options. Verify your insurance in 2 minutes (no obligation) → Start benefits check or call 561-203-6085. If you’re in crisis, call/text 988.