Spotting the Signs: A Deep Dive into PTSD’s DSM-5 Checklist

Why Understanding the PTSD DSM-5 Criteria Is the First Step Toward Getting Help
Disclaimer: This article discusses trauma, suicide, and other sensitive topics. If you are in crisis or experiencing suicidal thoughts, please call or text the 988 Suicide & Crisis Lifeline at 988. You are not alone.

If you’re searching for information about the ptsd dsm 5 criteria, you likely need clear answers about whether what you’re experiencing might be Post-Traumatic Stress Disorder. Understanding the diagnostic criteria isn’t just clinical jargon—it’s the roadmap mental health professionals use to identify PTSD and determine the right level of care.
The DSM-5 criteria for PTSD require:
- Criterion A: Exposure to actual or threatened death, serious injury, or sexual violence
- Criterion B: At least 1 intrusion symptom (unwanted memories, nightmares, flashbacks)
- Criterion C: At least 1 avoidance symptom (avoiding trauma-related thoughts or reminders)
- Criterion D: At least 2 negative alterations in cognitions and mood (persistent negative beliefs, guilt, detachment)
- Criterion E: At least 2 alterations in arousal and reactivity (irritability, hypervigilance, sleep problems)
- Criterion F: Symptoms lasting more than 1 month
- Criterion G: Symptoms causing significant distress or impairment in daily functioning
- Criterion H: Symptoms not attributable to substances or other medical conditions
Here’s what many people don’t realize: PTSD isn’t just about the traumatic event itself. It’s about how your brain and body respond afterward—sometimes immediately, sometimes months or even years later. The DSM-5 criteria exist to capture these complex patterns and ensure people get the right diagnosis and treatment, not guesswork.
A formal PTSD diagnosis can feel scary, but it’s actually empowering. It validates your experience, explains why you’re struggling, and opens the door to evidence-based treatments that genuinely work. Whether you’re dealing with intrusive flashbacks, constant hypervigilance, or feeling emotionally numb, knowing where you stand is the first step toward reclaiming your life.
As Nate Raine, CEO of Thrive Mental Health, I’ve spent over a decade at the intersection of behavioral health and evidence-based care, helping build systems that translate diagnostic frameworks like the ptsd dsm 5 criteria into real-world treatment pathways. Understanding these criteria isn’t just academic—it’s how we connect people in Florida to the right level of support, whether that’s intensive outpatient care, trauma-focused therapy, or hybrid treatment models designed for busy lives.
Basic ptsd dsm 5 criteria glossary:
What Counts as “Trauma”? Unpacking Criterion A
Before any other symptoms can be considered, the ptsd dsm 5 criteria demand a clear understanding of the “stressor” event itself. This is Criterion A, and it’s stricter than you might think. It’s not just any difficult experience, but specific types of events that involve actual or threatened death, serious injury, or sexual violence.
Exposure to such a traumatic event can happen in four distinct ways:
- Directly experiencing the traumatic event(s). This is the most straightforward: you were there, it happened to you.
- Witnessing, in person, the event(s) as it occurred to others. This means seeing someone else undergo the trauma firsthand.
- Learning that the traumatic event(s) occurred to a close family member or close friend. For this to count, the event must have been violent or accidental, not a natural death from illness.
- Experiencing repeated or extreme exposure to aversive details of the traumatic event(s). This usually applies to professionals like first responders, police officers, or military personnel who are regularly exposed to graphic details of human suffering. For example, a first responder collecting human remains or a police officer repeatedly exposed to details of child abuse could meet this criterion. Notably, this criterion specifically excludes exposure through electronic media, television, movies, or pictures unless it is work-related.
This strict definition ensures that the diagnosis is tied to events that typically overwhelm an individual’s coping mechanisms, setting it apart from other stress-related conditions.

You can explore the full diagnostic criteria for PTSD, including Criterion A, as outlined by the National Center for Biotechnology Information (NCBI) here: Exhibit 1.3-4, DSM-5 Diagnostic Criteria for PTSD – NCBI – NIH.
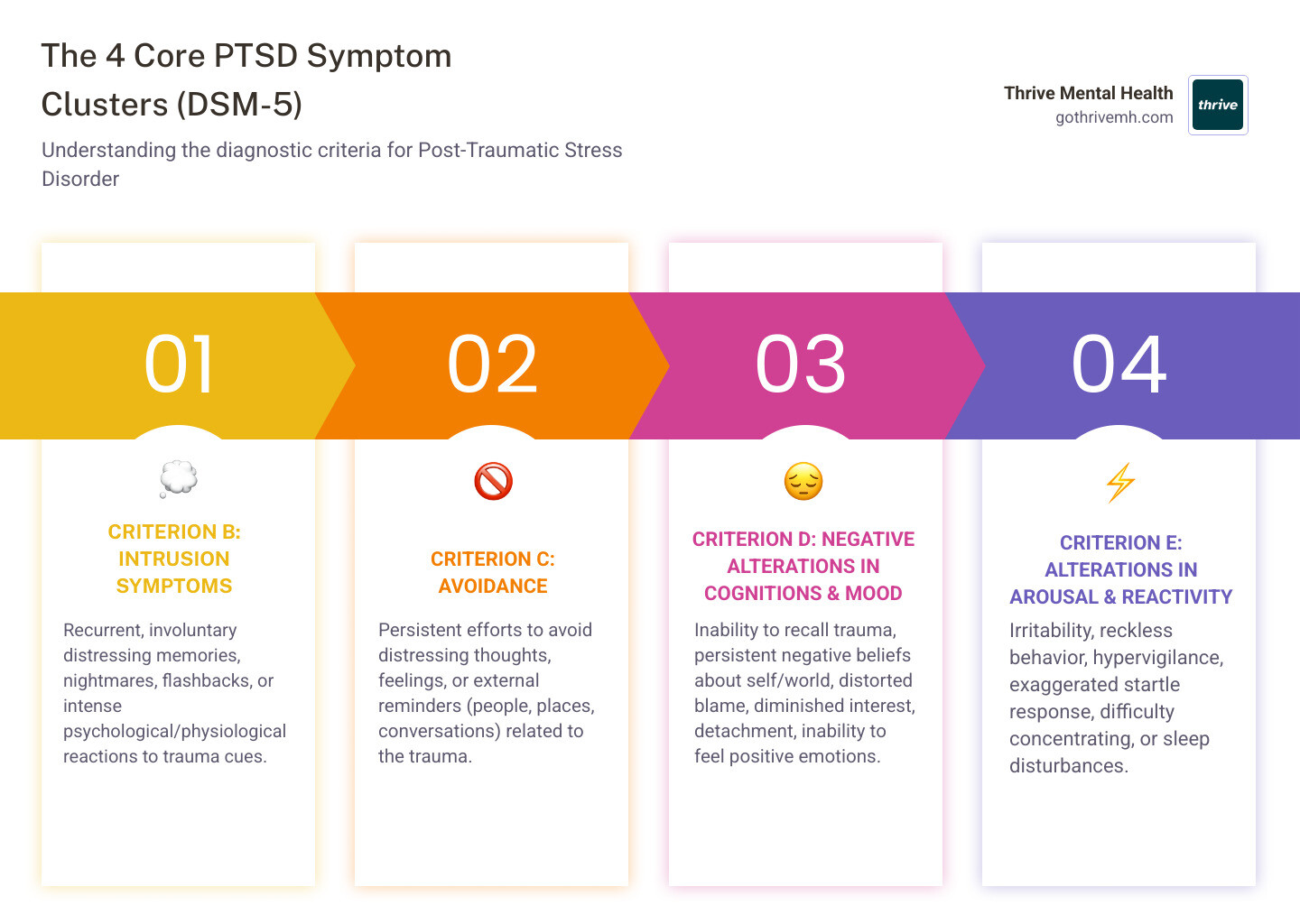
The 4 Core Symptom Clusters of the PTSD DSM-5 Criteria
Once a traumatic event (Criterion A) is established, the ptsd dsm 5 criteria then look for persistent symptoms across four distinct clusters. These aren’t just isolated feelings; they’re patterns of distress that significantly impact daily life. To receive a diagnosis, an individual must meet specific symptom counts within each of these categories.
Criterion B: Intrusive Memories That Won’t Fade
These are the “re-experiencing” symptoms – the trauma forcing its way back into your mind, often against your will. You need to experience at least one of the following five symptoms:
- Recurrent, involuntary, and intrusive distressing memories of the traumatic event(s). These aren’t just recollections; they’re vivid, upsetting memories that feel like they’re happening now. For children, this might manifest as repetitive play expressing themes of the trauma.
- Recurrent distressing dreams in which the content and/or affect of the dream are related to the traumatic event(s). Nightmares can be incredibly vivid and disturb sleep, often mirroring the fear or helplessness of the original event.
- Dissociative reactions (e.g., flashbacks) in which the individual feels or acts as if the traumatic event(s) were recurring. Flashbacks can range from brief moments of feeling detached to a complete loss of awareness, where you genuinely believe you’re reliving the trauma.
- Intense or prolonged psychological distress at exposure to internal or external cues that symbolize or resemble an aspect of the traumatic event(s). Triggers can be anything from a loud noise to a specific smell, instantly bringing back the emotional pain.
- Marked physiological reactions to internal or external cues that symbolize or resemble an aspect of the traumatic event(s). This means your body reacts as if in danger, with symptoms like a racing heart, sweating, or trembling, even when safe.
Criterion C: The Drive to Avoid Reminders
It’s natural to want to avoid pain, and for those with PTSD, this avoidance becomes a central coping mechanism. However, it often hinders healing. You need to experience at least one of the following two symptoms:
- Avoidance of or efforts to avoid distressing memories, thoughts, or feelings about or closely associated with the traumatic event(s). This is internal avoidance—trying to suppress painful thoughts or emotions.
- Avoidance of or efforts to avoid external reminders (people, places, conversations, activities, objects, situations) that arouse distressing memories, thoughts, or feelings about or closely associated with the traumatic event(s). This is external avoidance—actively steering clear of anything that might trigger a memory, such as avoiding driving after a car accident or staying away from social gatherings if the trauma occurred in a public place.
While avoidance offers short-term relief, it can reinforce the impact of PTSD and prevent individuals from processing their experiences. If you find yourself consistently avoiding trauma-related cues, it might be time to seek support. You can find more information about our Florida trauma care programs designed to help you steer these challenges: More info about our trauma care programs.
Criterion D: Negative Shifts in Thoughts and Mood
Trauma can fundamentally alter how you see yourself, others, and the world. These changes often lead to persistent negative emotional states. You need to experience at least two of the following seven symptoms:
- Inability to remember an important aspect of the traumatic event(s) (typically dissociative amnesia, not due to head injury, alcohol, or drugs). This isn’t just forgetting minor details but significant portions of the event.
- Persistent and exaggerated negative beliefs or expectations about oneself, others, or the world (e.g., “I am bad,” “No one can be trusted,” “The world is completely dangerous”).
- Persistent, distorted cognitions about the cause or consequences of the traumatic event(s) that lead the individual to blame himself/herself or others. This can involve intense guilt or shame.
- Persistent negative emotional state (e.g., fear, horror, anger, guilt, or shame). These emotions become pervasive and difficult to shake.
- Markedly diminished interest or participation in significant activities. This is often referred to as anhedonia, a loss of pleasure in things once enjoyed.
- Feelings of detachment or estrangement from others. You might feel isolated, even when surrounded by loved ones.
- Persistent inability to experience positive emotions (e.g., inability to experience happiness, satisfaction, or loving feelings). This emotional numbness can be a profound and painful symptom.
Criterion E: Arousal and Reactivity on High Alert
After trauma, your nervous system can remain in a constant state of alert, making it difficult to relax or feel safe. You need to experience at least two of the following six symptoms:
- Irritable behavior and angry outbursts (with little or no provocation) typically expressed as verbal or physical aggression toward people or objects.
- Reckless or self-destructive behavior. This could include excessive risk-taking or engaging in harmful activities.
- Hypervigilance. You’re constantly scanning your environment for threats, always on edge and expecting danger.
- Exaggerated startle response. Even minor unexpected noises or movements can cause an intense physical reaction.
- Problems with concentration. It becomes difficult to focus on tasks, conversations, or even simple activities.
- Sleep disturbance (e.g., difficulty falling or staying asleep or restless sleep). Insomnia or frequent awakenings are common.
Finalizing the Diagnosis: Timing, Impairment, and Critical Specifiers
The ptsd dsm 5 criteria go beyond just the types of symptoms; they also consider how long these symptoms last, their impact on your life, and any unique ways they might manifest. These additional criteria are crucial for a precise diagnosis.

How long must symptoms last for a PTSD diagnosis? (Criteria F & G)
The duration and impact of symptoms are non-negotiable for a PTSD diagnosis.
- Criterion F: Duration. The disturbance, encompassing symptoms from Criteria B, C, D, and E, must last for more than 1 month. This differentiates PTSD from Acute Stress Disorder, which has similar symptoms but resolves within a month.
- Criterion G: Functional Significance. The symptoms must cause clinically significant distress or impairment in social, occupational, or other important areas of functioning. This means your symptoms aren’t just inconvenient; they’re actively interfering with your relationships, work, school, or overall quality of life. Without this impairment, a diagnosis isn’t warranted, even if some symptoms are present.
Ruling Out Other Causes (Criterion H)
To ensure an accurate diagnosis, mental health professionals must rule out other potential explanations for your symptoms. This is Criterion H:
- The disturbance is not attributable to the physiological effects of a substance (e.g., medication, alcohol) or another medical condition. It’s essential to ensure that symptoms aren’t a side effect of medication, substance use, or an underlying physical health issue. This step helps prevent misdiagnosis and ensures you receive the most appropriate treatment.
What are the Dissociative and Delayed Specifiers for the ptsd dsm 5 criteria?
The DSM-5 includes important “specifiers” that provide a more nuanced description of PTSD, indicating particular symptom patterns or timing.
- With Dissociative Symptoms: This specifier applies if, in addition to meeting the general PTSD criteria, an individual experiences high levels of either:
- Depersonalization: Persistent or recurrent experiences of feeling detached from one’s mental processes or body, as if one is an outside observer of oneself (e.g., feeling as if “this is not happening to me,” or being in a dream).
- Derealization: Persistent or recurrent experiences of unreality of surroundings (e.g., the world around the individual is experienced as unreal, dreamlike, distant, or distorted).
These dissociative symptoms are often a response to trauma-related stimuli. The U.S. Department of Veterans Affairs (VA) provides more detailed information on this subtype: Dissociative Specification explained by the VA.
- With Delayed Expression: This specifier is used if the full diagnostic criteria for PTSD are not met until at least six months after the traumatic event(s), even though some symptoms may have appeared earlier. This acknowledges that for some individuals, the full impact of trauma can take time to manifest.
How the DSM-5 Changed PTSD Diagnosis (And Why It Matters)
The DSM-5, published in 2013, brought significant revisions to the ptsd dsm 5 criteria, marking an evolution in how mental health professionals understand and diagnose trauma-related conditions. These changes weren’t arbitrary; they were based on extensive research and clinical experience, aiming for greater accuracy and clinical utility.
One of the most notable shifts was moving PTSD from the “Anxiety Disorders” chapter into a new category: Trauma- and Stressor-Related Disorders. This emphasized that exposure to a traumatic or stressful event is a prerequisite for diagnosis, distinct from other anxiety conditions.
Here’s a breakdown of other key changes from the previous version, DSM-IV:
- Criterion A2 Removal: The DSM-IV required an “intense fear, helplessness, or horror” response during the traumatic event (Criterion A2). This was removed in the DSM-5 because research showed it didn’t improve diagnostic accuracy and sometimes excluded individuals who had a delayed emotional reaction or couldn’t express these feelings.
- Splitting Avoidance and Numbing: In DSM-IV, avoidance and emotional numbing were combined into one cluster. The DSM-5 separated these into two distinct criteria:
- Criterion C (Avoidance): Focused specifically on efforts to avoid trauma-related thoughts, feelings, or external reminders.
- Criterion D (Negative Alterations in Cognitions and Mood): Became its own cluster, incorporating symptoms of emotional numbing, persistent negative beliefs, distorted blame, and inability to experience positive emotions. This expanded the understanding of how trauma impacts a person’s inner world.
- Addition of New Symptoms: The DSM-5 introduced three new symptoms to better capture the full range of PTSD experiences:
- Persistent negative beliefs/assumptions about oneself, others, or the world.
- Persistent negative affect (emotional state).
- Reckless or self-destructive behavior.
Overall, the DSM-5 now lists 20 potential symptoms, an increase from the 17 in DSM-IV.
- Preschool Subtype: The DSM-5 introduced a specific set of criteria for PTSD in children aged six years and younger, recognizing that trauma manifests differently in very young children.
- Impact on Prevalence Rates: While the changes were significant, national estimates suggest the revisions had a minimal impact on overall PTSD prevalence rates, typically resulting in about a 1% lower prevalence compared to DSM-IV. This indicates the DSM-5 refined the diagnosis without drastically altering who qualifies for it.
Here’s a quick comparison of the key differences:
| Feature | DSM-IV PTSD Criteria | DSM-5 PTSD Criteria (The DSM-5 criteria for PTSD are extensive and require a specific combination of symptoms, not all 20 are needed for diagnosis).
From Diagnosis to Recovery: Getting Evidence-Based Treatment That Works
A PTSD diagnosis, guided by the ptsd dsm 5 criteria, is not a life sentence. It’s a call to action. We know that with the right treatment, recovery is not just possible—it’s probable. Clinical trials consistently show that evidence-based therapies are highly effective in alleviating symptoms over the long term.
At Thrive Mental Health, we believe in a holistic, personalized approach to healing. Our programs are designed to meet you where you are, offering the intensive support you need to reclaim your life.
Key treatment approaches that align with the DSM-5 framework include:
- Psychotherapy: Often the first line of defense, talk therapy helps individuals process their traumatic experiences and develop healthier coping mechanisms.
- Cognitive Behavioral Therapy (CBT): This widely recognized therapy helps you identify and change negative thought patterns and behaviors contributing to PTSD symptoms. For instance, a therapist might help you challenge the belief that “the world is completely dangerous,” which fuels hypervigilance.
- Prolonged Exposure Therapy (PE): A specific type of CBT, PE gradually exposes you to trauma-related memories, feelings, and situations in a safe environment, helping you process and reduce your fear response.
- Eye Movement Desensitization and Reprocessing (EMDR): This innovative therapy helps you process traumatic memories by focusing on external stimuli (like eye movements) while recalling the event. Research suggests EMDR can be more effective than CBT for reducing the severity of adverse emotions and memories surrounding trauma.
- Somatic Experiencing (SE): This body-oriented therapy focuses on how trauma impacts the nervous system and physical sensations. By gently guiding you to notice and release trapped energy in the body, SE can help reduce chronic pain, headaches, and physical illnesses often associated with unresolved trauma.
- Intensive Outpatient Programs (IOP) and Partial Hospitalization Programs (PHP): For many, once-a-week therapy isn’t enough. Our virtual and hybrid IOP/PHP programs offer structured, comprehensive care that fits into your life. These programs provide a higher level of support than traditional outpatient therapy but less than inpatient care, making them ideal for individuals who need intensive treatment while maintaining daily responsibilities. You can learn more about our intensive virtual care options here: Virtual IOP programs for trauma and explore our robust Partial Hospitalization Programs (PHP).
- Medication: While not a standalone solution, certain medications, such as selective serotonin reuptake inhibitors (SSRIs), can help manage severe symptoms like anxiety, depression, and sleep disturbances, creating a foundation for therapy to be more effective. Always consult a doctor before starting or changing any medication.
We understand that accessing quality mental healthcare is crucial. That’s why Thrive Mental Health offers virtual and hybrid programs across Florida. We work with major insurance providers like Cigna, Optum, and Florida Blue to ensure our evidence-based treatments are accessible. Don’t let financial concerns hold you back from getting the care you deserve.
Frequently Asked Questions about the PTSD DSM-5 Criteria
What are the 20 symptoms of PTSD in the DSM-5?
The DSM-5 identifies a total of 20 distinct symptoms across four clusters: Intrusion (5 symptoms), Avoidance (2 symptoms), Negative Alterations in Cognitions/Mood (7 symptoms), and Alterations in Arousal/Reactivity (6 symptoms). A diagnosis requires a specific combination of these symptoms, not necessarily all 20. For example, you need at least one from the Intrusion cluster, one from Avoidance, two from Negative Alterations, and two from Arousal/Reactivity, along with duration and impairment criteria.
Can you be diagnosed with PTSD if symptoms appear years later?
Yes. This is known as PTSD with delayed expression (or delayed onset). The full diagnostic criteria are not met until at least six months after the traumatic event, though some initial symptoms may have appeared earlier. This highlights that the impact of trauma can manifest over time, and it’s never too late to seek help.
What’s the difference between PTSD and Complex PTSD (C-PTSD)?
While C-PTSD is not an official diagnosis in the DSM-5, it is a widely recognized term in clinical practice and research. It describes a more severe and pervasive form of PTSD resulting from prolonged, repeated trauma, often in childhood (e.g., ongoing abuse, neglect, captivity). C-PTSD includes the standard PTSD symptoms plus additional difficulties with emotional regulation, self-concept (e.g., pervasive feelings of shame or worthlessness), and interpersonal relationships (e.g., difficulty forming secure attachments or trusting others).
Are there different PTSD criteria for children?
Yes, the DSM-5 has a separate set of criteria for children aged six and younger. These criteria account for developmental differences, as young children may express trauma differently than adults. For instance, distressing memories might manifest as repetitive play expressing themes of the event, or recurrent distressing dreams might occur without recognizable content.
Your Diagnosis Is Not Your Destiny
A formal diagnosis using the ptsd dsm 5 criteria is the critical first step toward understanding your experiences and accessing effective care. While the symptoms can feel overwhelming, recovery is possible with the right support. Thrive Mental Health offers expert-led, evidence-based programs designed to help you process trauma and build a life you value.
Ready for support? Thrive offers virtual and hybrid IOP/PHP programs with evening options for Florida residents. Verify your insurance in 2 minutes (no obligation) → Start benefits check. If you’re in crisis, call/text 988.