CBT for Depression: An Effective Strategy for Managing Moods
Your First Step Away from Depression’s Grip
CBT for depression is one of the most effective, evidence-based treatments available—helping you challenge negative thoughts, rebuild healthy behaviors, and regain control of your mood. Whether you’re struggling with persistent sadness, loss of motivation, or hopelessness, Cognitive Behavioral Therapy offers practical tools to break free from depression’s grip.
What You Need to Know About CBT for Depression:
- What it is: A structured, goal-oriented talk therapy that teaches you to identify and change unhelpful thinking patterns and behaviors that fuel depression.
- How effective it is: About 75% of people who receive CBT for depression improve, with symptoms often reduced by half or more.
- How it compares to medication: CBT is as effective as antidepressants for mild to moderate depression, with lower relapse rates and more lasting effects.
- How long it takes: Most people see meaningful improvements within 8-16 sessions, depending on severity.
- Who it helps: CBT works for people of all ages—from adolescents to older adults—and is effective for mild, moderate, and severe depression (especially when combined with medication for severe cases).
Depression doesn’t just drain your energy—it warps how you see yourself, your world, and your future. You might feel stuck in a cycle of negative thoughts, isolation, and behaviors that make everything worse. CBT breaks that cycle by teaching you to rewire your brain’s negative loops through practical, skill-based strategies.
Unlike medication alone, CBT gives you tools you can use for life. It’s not about “positive thinking”—it’s about learning to question distorted thoughts, test them against reality, and take action even when motivation feels impossible. Research shows that CBT not only reduces symptoms but also helps prevent relapse better than medication alone.
I’m Nate Raine, CEO of Thrive Mental Health, where we’ve built evidence-based programs that integrate CBT for depression into flexible, virtual IOP and PHP settings. We are proud to offer these services to residents throughout Florida, as well as in California, Arizona, Indiana, and South Carolina. Throughout my career leading behavioral health innovation, I’ve seen how CBT for depression transforms lives by giving people the skills to manage their moods and reclaim their sense of control.
Know your cbt for depression terms:
What is CBT and Why is it a Go-To for Depression?
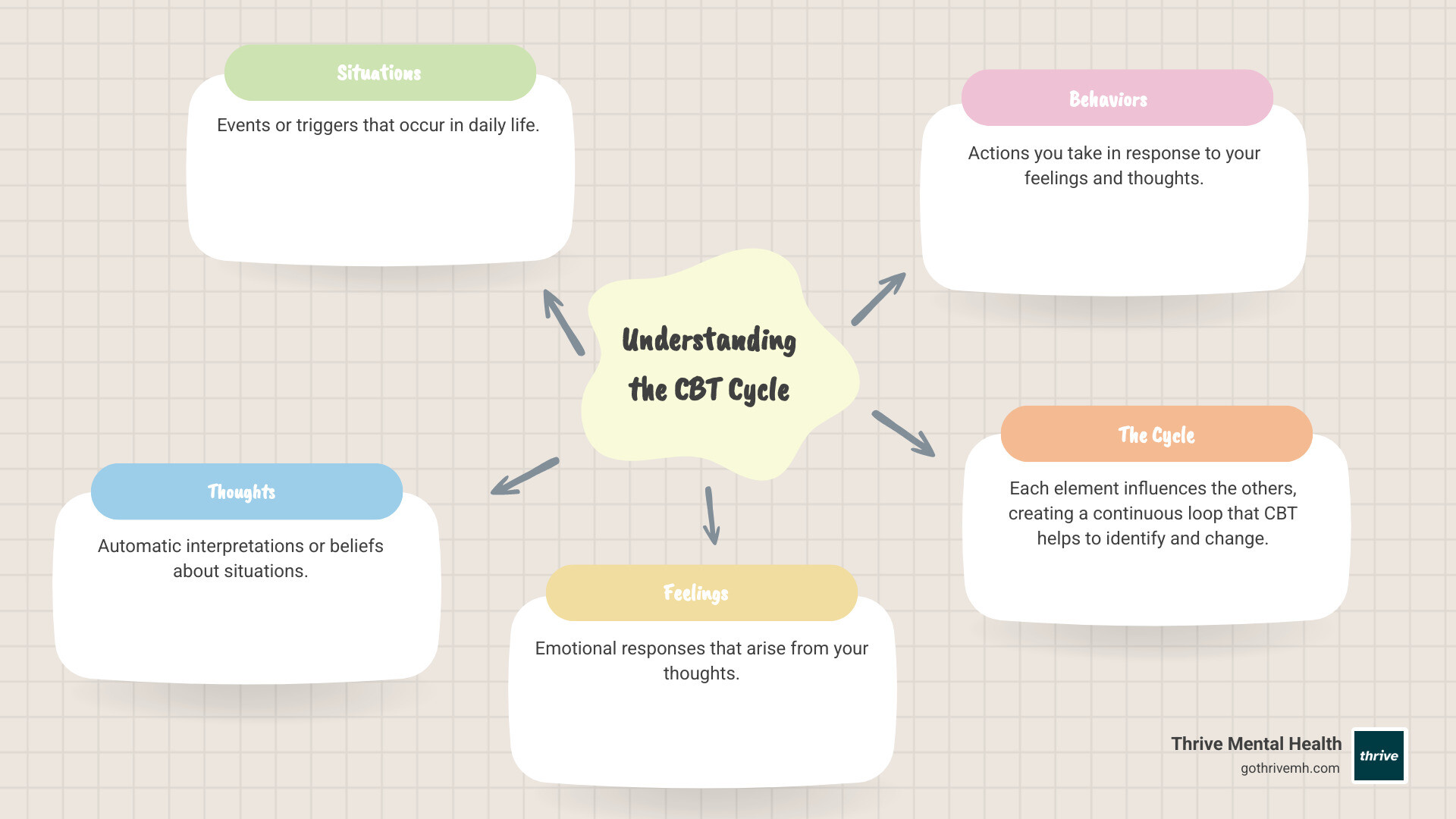
Cognitive Behavioral Therapy (CBT) is a structured, goal-oriented type of talk therapy that helps people manage mental health conditions and emotional concerns. It’s based on the powerful idea that our thoughts, feelings, and behaviors are all interconnected. By learning to identify and change unhelpful thinking patterns and learned behaviors, we can dramatically improve how we feel.
Developed by Dr. Aaron Beck, CBT for depression is not just another therapy; it’s often considered the gold standard of psychotherapy due to its extensive evidence base. Its core principles revolve around understanding that psychological issues often stem from problematic ways of thinking and behaving, and that we can actively learn better coping mechanisms. This empowers us to relieve symptoms and improve our overall mental well-being.
The Core Idea: You Can Change How You Feel by Changing How You Think
At the heart of CBT for depression is the cognitive model. This model proposes that it’s not simply events themselves that upset us, but rather our interpretation or view of those events. For example, if you spill coffee, the event itself isn’t inherently catastrophic, but a thought like “I always mess everything up” can trigger feelings of sadness or frustration, leading to behaviors like withdrawal or self-criticism.
This creates a “vicious cycle” where maladaptive thinking processes and negative appraisals lead to dysfunctional cognitive reactions, which in turn cause depressive symptoms in our emotions and behaviors. CBT for depression teaches us how to identify these cycles and intervene, breaking them down into manageable parts. It’s about recognizing that you have the power to change how you react and respond, fostering empowerment and building essential life skills.
How CBT Specifically Targets Depression Symptoms
Depression manifests in many ways, from persistent sadness and hopelessness to physical symptoms and behavioral changes. CBT for depression is uniquely equipped to tackle these varied symptoms by addressing their underlying cognitive and behavioral patterns.
For instance, depression often brings:
- Anhedonia: A loss of interest or pleasure in activities once enjoyed.
- Low motivation: A pervasive feeling of lethargy that makes even simple tasks feel overwhelming.
- Negative self-talk: A constant inner critic that reinforces feelings of worthlessness.
- Hopelessness: A belief that things will never get better.
- Isolation: A tendency to withdraw from social interactions and activities.
We use CBT for depression to target these specific challenges. We help you understand how these patterns develop and, more importantly, how to interrupt them. By addressing the root cognitive and behavioral patterns, we can empower you to counteract the effects of depression symptoms and regain a sense of control over your life.
How CBT for Depression Rewires Your Brain’s Negative Loops
CBT for depression is not a passive process; it’s an active collaboration between you and your therapist. It’s about learning and applying practical techniques, often through “homework” assignments between sessions, to rewire the negative loops that keep depression entrenched. This active participation is crucial for making lasting changes.
Our approach focuses on giving you actionable strategies. We work together to help you identify, challenge, and ultimately change the thoughts and behaviors that contribute to your depression. This process is deeply empowering, as you learn to be your own therapist in the long run. To learn more about this, explore How CBT Can Transform Negative Thought Patterns.
Cognitive Restructuring: Challenging and Changing Your Thoughts
One of the cornerstones of CBT for depression is cognitive restructuring. This technique helps you identify and challenge what we call Automatic Negative Thoughts (ANTs)—those spontaneous, often negative thoughts that pop into our heads and influence our mood and behavior. These ANTs often stem from cognitive distortions, which are biased or irrational ways of interpreting information.
Common cognitive distortions include:
- Black-and-white thinking: Seeing things in extremes (“If I don’t top the exams, I’m a failure.”).
- Fortune-telling: Predicting negative outcomes without evidence (“I’ll be so upset, I won’t be able to function at all.”).
- Disqualifying the positive: Ignoring positive experiences (“I cracked the exam, but that doesn’t mean I’m competent; it was a fluke.”).
- Emotional reasoning: Believing something is true because you feel it strongly (“I know I successfully complete most of my tasks, but I still feel like I’m incompetent.”).
- Overgeneralization: Drawing broad negative conclusions from a single event (“Because I felt uncomfortable at the meeting, I don’t have what it takes to be a group leader.”).
We use tools like thought records, where you document upsetting situations, your automatic thoughts, and the emotions they trigger. Then, through a process called Socratic questioning and guided findy, we help you examine the evidence for and against your thoughts, consider alternative perspectives, and develop more balanced and realistic thoughts. This process helps you recognize distorted thinking and replace it with constructive, healthier perspectives.
Behavioral Activation: Taking Action to Break the Cycle
While cognitive restructuring tackles thoughts, behavioral activation addresses the behavioral side of depression. Depression often leads to withdrawal and inactivity, which further fuels negative thoughts and feelings, creating a downward spiral. Behavioral activation aims to reverse this by encouraging you to engage in activities, even when you don’t feel motivated.
We work with you to identify and schedule activities that bring a sense of pleasure or mastery. This could be anything from taking a short walk (pleasure) to completing a small task you’ve been putting off (mastery). The goal is not to wait until you feel like doing something, but to do something to change how you feel. By proactively engaging in life, you start to overcome inertia, build positive momentum, and gradually re-engage with the world in a way that counters depressive patterns. This is a powerful way to shift your mood and energy, proving that action can precede motivation.
CBT vs. Medication: What the Evidence Shows for Lasting Relief
When it comes to treating depression, both CBT for depression and medication are highly effective, and often, the best approach involves a combination of both. However, understanding their individual strengths and long-term benefits can help you make an informed decision about your treatment path.

The evidence base supporting CBT for depression is robust. Numerous studies and meta-analyses consistently demonstrate its effectiveness, often highlighting its lasting impact and ability to reduce relapse rates.
The Science-Backed Effectiveness of CBT for Depression
We know that CBT for depression works. Statistics show that about 75% of people who receive CBT for depression treatment improve, with symptoms typically reduced by about half. This makes it a formidable treatment option. Research and reviews done by the NCBI consistently point to CBT as one of the most effective evidence-based therapeutic interventions for depression.
For mild to moderate depression, CBT for depression is often recommended as a first-line treatment and has been found to be as effective as medication. For more severe or chronic depression, the combination of CBT and antidepressants is often the most powerful strategy, leading to faster remission and better outcomes. Even for treatment-resistant depression, CBT can be a crucial component, especially after initial medication trials haven’t yielded sufficient results.
Here’s a comparison of CBT, antidepressants, and combined treatment:
| Treatment Type | Benefits | Limitations | Best For |
|---|---|---|---|
| CBT (alone) | Teaches coping skills for life, lasting effects, lower relapse rates, non-pharmacological, no side effects like medication | Requires active participation and commitment, may not be sufficient for severe depression, access to qualified therapists can be an issue | Mild to moderate depression, relapse prevention, individuals preferring non-medication approaches |
| Antidepressants (alone) | Rapid symptom relief, effective for moderate to severe depression, can stabilize mood quickly | Potential side effects (nausea, weight gain, sexual dysfunction), withdrawal symptoms upon discontinuation, doesn’t teach coping skills, higher relapse rates after stopping | Moderate to severe depression, quick symptom management, when CBT alone is insufficient |
| Combined Treatment (CBT + Antidepressants) | Most effective for severe/chronic depression, faster remission, significantly better relapse prevention, addresses both symptoms and underlying patterns | Potential side effects from medication, higher cost than monotherapy, requires coordination between providers, may involve more appointments | Severe or chronic depression, treatment-resistant depression, individuals seeking comprehensive and robust recovery |
The Long Game: Why CBT Is a Powerful Tool for Relapse Prevention
One of the most significant advantages of CBT for depression is its long-term impact, particularly concerning relapse prevention. While antidepressants can alleviate symptoms, they don’t inherently equip you with coping skills. When medication is discontinued, relapse rates can be high.
In contrast, CBT for depression teaches you practical skills to manage your thoughts and behaviors, making you more self-sufficient in the face of future stressors. Studies have shown that CBT is linked to lower relapse rates compared to medication alone. For example, one study found that only 29.5% of patients treated with cognitive therapy relapsed, compared with 60% of those treated with antidepressants. This means you gain a toolkit you can use for life, reducing the likelihood of future depressive episodes.
To further bolster long-term resilience, maintenance sessions or “booster sessions” can be incorporated after initial treatment to reinforce learned skills and address any emerging challenges, ensuring the benefits of CBT endure.
Finding Your Fit: Individual, Group, and Virtual CBT Options
Accessing CBT for depression has become more flexible than ever, with various formats designed to meet diverse needs and preferences. Whether you prefer one-on-one attention, the support of a group, or the convenience of virtual care, we offer options that make evidence-based treatment accessible.
At Thrive Mental Health, we are dedicated to making CBT for depression accessible to residents throughout Florida. Our virtual programs are available statewide, and we work with major insurance providers, including Florida Blue, Cigna, Optum, and Aetna, to help cover the cost of care. We also serve clients in California, Indiana, Arizona, and South Carolina.
Individual vs. Group Therapy: Which is Right for You?
The choice between individual and group CBT for depression often depends on your personal needs and comfort level:
- Individual CBT: This offers one-on-one attention, allowing for highly personalized treatment custom specifically to your unique challenges and goals. It provides a private space to explore sensitive issues and receive undivided focus from your therapist.
- Group CBT: This format provides a powerful sense of peer support and shared experience. Hearing from others facing similar struggles can normalize your feelings and reduce isolation, which is a common symptom of depression. Group therapy is often more cost-effective and can provide a supportive community that reinforces learning.
While computerized CBT (cCBT) programs are available, research suggests they may not be as effective as traditional therapist-led CBT due to low uptake and engagement, especially without significant clinical support. We prioritize human-centered, expert-led care to ensure you get the best results.
The Rise of Virtual CBT: Getting Help from Anywhere
The advent of virtual care has revolutionized access to CBT for depression. Virtual Cognitive Behavioral Therapy: Complete Guide highlights how this format breaks down geographic barriers. For residents across Florida—from Miami to the Panhandle—this means you can receive high-quality care from the comfort of your home or office, without worrying about traffic or travel. This flexibility is particularly beneficial for working professionals or anyone who might face challenges with in-person appointments.
Our virtual Intensive Outpatient Programs (IOPs) provide structured, comprehensive care that integrates CBT for depression. These programs are designed for individuals who need more support than traditional weekly therapy but less than inpatient hospitalization. They offer a flexible schedule, often with evening options, making it easier to balance treatment with work and family commitments. Explore our Intensive Outpatient Programs for Depression to see if this is the right fit for you.
Frequently Asked Questions about CBT for Depression
How long does CBT for depression take to work?
CBT for depression is generally considered a short-term therapy. The typical course of treatment can range from 8 to 16 sessions, with each session lasting about 45 minutes to an hour. For mild depression, 8-12 sessions might be sufficient, while moderate depression often requires 8-16 sessions. Severe or chronic depression may need 16 or more sessions, sometimes followed by “booster sessions” for up to 1-2 years to prevent relapse. Many individuals begin to notice improvements in their mood and overall well-being within a few weeks of consistent engagement.
Is CBT effective for all types of depression?
CBT for depression is highly effective for a wide range of depressive disorders. It’s often recommended as a first-line treatment for mild to moderate major depressive disorder (MDD) and situational depression. For severe or chronic depression, it’s frequently most effective when combined with medication. CBT is also a valuable tool for specific populations, such as individuals with postpartum depression, adolescents with mild to moderate depression, and adults experiencing depression alongside chronic medical conditions.
What happens if CBT doesn’t work for me?
While CBT for depression has a high success rate, no single therapy works for everyone. If you’re not experiencing the progress you hoped for, it’s important to discuss this with your therapist. Factors like the therapeutic alliance (your relationship with your therapist) can significantly impact outcomes. Options include trying a different therapist who might be a better fit, combining CBT with medication if you haven’t already, or exploring other evidence-based therapies like Dialectical Behavior Therapy (DBT) or Eye Movement Desensitization and Reprocessing (EMDR). We believe in finding the right approach for your unique needs.
Take Control of Your Mood with Expert-Led CBT
At Thrive Mental Health, we integrate the proven power of CBT for depression into our flexible, expert-led virtual IOP programs, available to all residents of Florida. Our programs are designed to provide the comprehensive support you need to get real, measurable results, helping you steer your path to mental wellness right from your home.
Ready for support in Florida? Thrive offers virtual IOP and PHP programs with evening options, accessible from anywhere in the state. Verify your insurance in 2 minutes (no obligation) → Start benefits check or call 561-203-6085. If you’re in crisis, call/text 988.
