Beyond PTSD: Understanding Complex Trauma

Complex Post Traumatic Stress Disorder: 6 Steps to Hope
Why Complex Post Traumatic Stress Disorder Goes Beyond Traditional PTSD
Complex post traumatic stress disorder (C-PTSD) affects an estimated 1-8% of the world’s population, yet many people have never heard of it. Unlike PTSD, which typically stems from a single traumatic event, C-PTSD develops from prolonged, repeated trauma—often starting in childhood.
What is Complex Post Traumatic Stress Disorder?
- A mental health condition caused by chronic, repeated trauma
- Includes all PTSD symptoms plus difficulties with emotions, relationships, and self-image
- Recognized in the World Health Organization’s ICD-11 (but not yet in the DSM-5)
- Often misdiagnosed as borderline personality disorder or depression
- Requires specialized, long-term treatment approaches
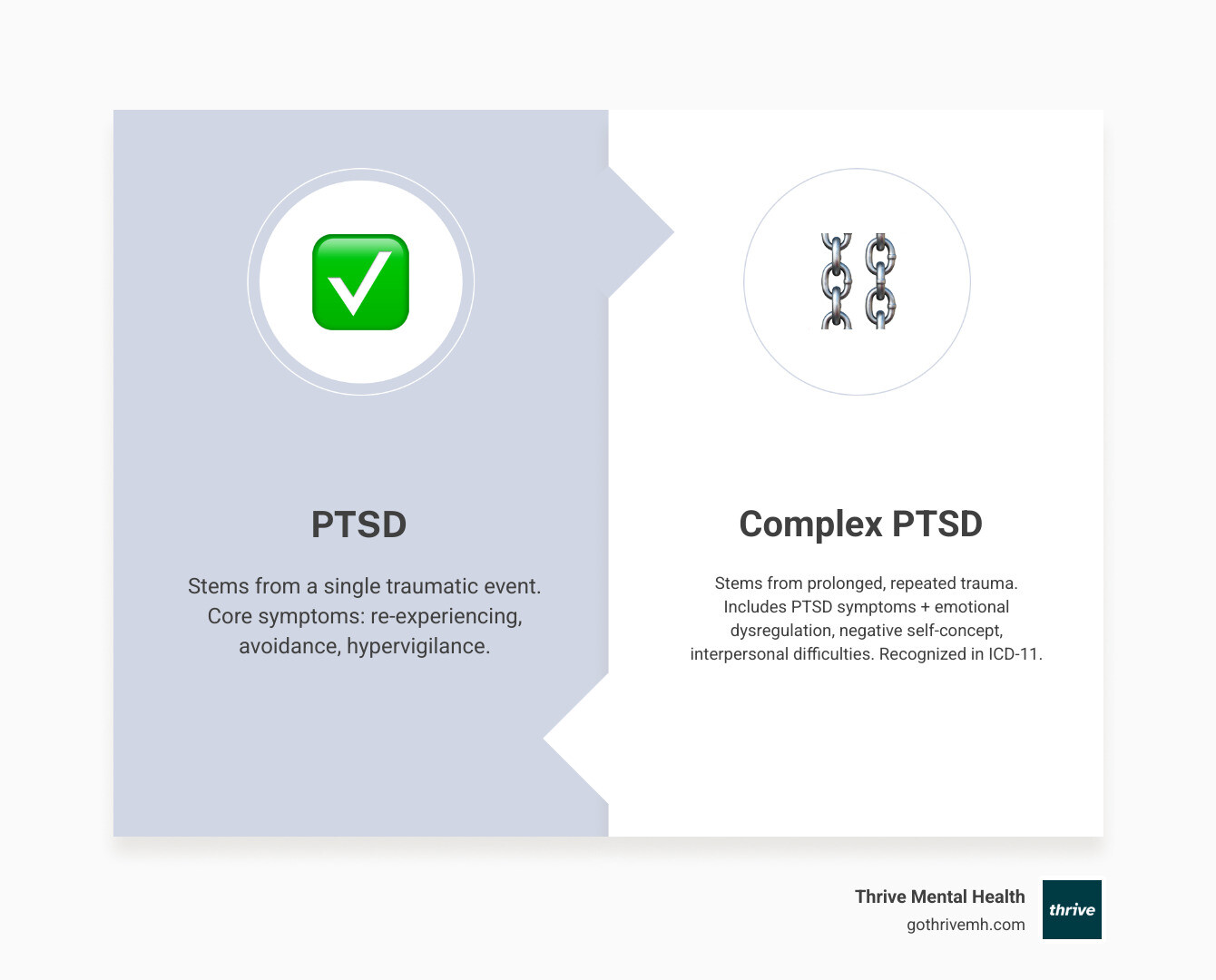
The key difference lies in the nature of the trauma. While PTSD might develop after a car accident, C-PTSD typically results from situations where escape felt impossible—like childhood abuse, domestic violence, or human trafficking. This prolonged exposure creates deeper changes in how someone sees themselves, manages emotions, and connects with others.
But here’s what matters most: recovery is possible. With proper understanding and trauma-informed care, people with C-PTSD can heal.
As Anna Green, LMHC, LPC, and founder of Thrive Mental Health, I specialize in treating complex trauma. My experience using evidence-based therapies like EMDR shows that while C-PTSD is challenging, the right approach leads to profound healing and growth.
Simple guide to complex post traumatic stress disorder:
What is Complex PTSD? [Key Differences, Symptoms & Diagnosis]
Disclaimer: If you or someone you know is in crisis or having thoughts of suicide, please call or text 988 to reach the Suicide & Crisis Lifeline. You are not alone.
Understanding complex post traumatic stress disorder is key to getting the right help. If PTSD is like a sudden injury from one event, C-PTSD is like repeated injuries that cause deeper damage to one’s sense of self and ability to connect with others.
Regular PTSD often follows a single event like a car accident or assault. Complex post traumatic stress disorder, on the other hand, stems from prolonged, repeated trauma that felt inescapable, such as childhood abuse or neglect, domestic violence, or human trafficking. These experiences, especially during developmental years, can fundamentally alter brain development.
ICD-11 vs. DSM-5: The Diagnostic Divide
The World Health Organization recognized complex post traumatic stress disorder in its ICD-11 manual, but the American Psychiatric Association’s DSM-5 has not. This means diagnosis can vary depending on the clinician, though many trauma specialists recognize C-PTSD as a distinct condition that isn’t fully captured by existing PTSD criteria.
Core Symptom Clusters: Beyond the Basics
Both PTSD and C-PTSD share core symptoms: flashbacks (re-experiencing), avoiding trauma reminders, and feeling on edge (hypervigilance). However, C-PTSD adds three layers of difficulty known as “Disturbances in Self-Organization”:
- Affect dysregulation: Intense mood swings, explosive anger, or emotional numbness.
- Negative self-concept: Deep feelings of shame, worthlessness, and believing you are fundamentally damaged.
- Relationship disturbances: Severe difficulty trusting others, maintaining boundaries, or feeling secure in relationships.
| Feature | Post-Traumatic Stress Disorder (PTSD) | Complex Post Traumatic Stress Disorder (C-PTSD) |
|---|---|---|
| Nature of Trauma | Single, distinct event(s) | Prolonged, repeated, often interpersonal trauma |
| Core PTSD Symptoms | Re-experiencing, avoidance, hypervigilance (primary focus) | Re-experiencing, avoidance, hypervigilance (present, but alongside broader challenges) |
| Emotional Regulation | May struggle with emotions related to trauma | Severe difficulties managing emotions across situations |
| Self-Perception | May question identity related to trauma | Profound feelings of worthlessness, shame, feeling “damaged” |
| Relationships | May avoid trauma-related relationships | Pervasive difficulties forming and maintaining healthy relationships |
| Diagnostic Recognition | Recognized in both DSM-5 and ICD-11 | Recognized in ICD-11; some symptoms covered under expanded PTSD in DSM-5 |
Diagnostic Challenges and Misdiagnosis
Accurately diagnosing complex post traumatic stress disorder is difficult because its symptoms overlap with other conditions, most commonly Borderline Personality Disorder (BPD). While both involve emotional and relationship difficulties, C-PTSD is directly rooted in chronic trauma. Research shows that C-PTSD qualifies as a separate disorder from BPD. Another area of confusion is traumatic grief, where loss occurs under traumatic circumstances. An accurate diagnosis requires a careful assessment of one’s trauma history and full range of symptoms, often using tools like the International Trauma Questionnaire (ITQ).
The 6 Core Symptoms of Complex PTSD
Beyond standard PTSD symptoms, C-PTSD involves six key areas of difficulty:
- Emotional dysregulation: Emotions feel out of control, leading to intense mood swings, explosive anger, or numbness. Your emotional thermostat feels broken.
- Interpersonal difficulties: Trust is incredibly challenging when caregivers caused harm. This can lead to pushing people away, fearing abandonment, or repeating unhealthy relationship patterns.
- Negative self-concept: A persistent inner critic tells you you’re worthless or damaged. It’s a deep-seated belief that you are irreparably different.
- Dissociation: A survival mechanism that involves feeling disconnected from yourself, your body, or reality. This can range from “spacing out” to out-of-body experiences.
- Alterations in attention: Difficulty concentrating, brain fog, and memory gaps (especially around traumatic events) are common.
- Somatic symptoms: Trauma lives in the body, causing chronic pain, headaches, or digestive issues with no clear medical cause. Research shows high rates of physical symptoms in people with complex PTSD.
How is Complex Post Traumatic Stress Disorder Diagnosed?
A diagnosis requires a mental health professional specializing in trauma. Since C-PTSD is not yet in the DSM-5, not all clinicians are familiar with it. A thorough assessment involves exploring your trauma history in detail and evaluating both core PTSD symptoms and the disturbances in self-organization. Clinicians may use the International Trauma Questionnaire (ITQ). A key part of the process is ruling out other conditions like BPD, though the chronic trauma history is a key differentiator for C-PTSD.
You can find more scientific research on Complex PTSD diagnosis to better understand the process.
The Roots of Complex Trauma: Causes & Risk Factors
Unlike the shock of a single event, complex post traumatic stress disorder develops from trauma that is prolonged, repetitive, interpersonal (caused by other people), and feels inescapable. This combination doesn’t just frighten someone—it fundamentally changes how they see themselves and the world.
Common causes include:
- Childhood abuse and neglect: When caregivers are the source of harm, it disrupts healthy development. Studies show that childhood trauma can significantly affect brain development, creating survival patterns that persist into adulthood.
- Domestic violence: The cycle of abuse keeps victims constantly on edge and trapped by barriers like financial dependence or threats. Research found that C-PTSD was twice as common in survivors of intimate partner violence compared to traditional PTSD.
- Human trafficking: This extreme form of trauma involves severe exploitation and captivity, combining physical harm with psychological manipulation. Approximately 41% of human trafficking survivors develop complex PTSD.
Other causes include torture, genocide and war experiences, long-term community violence, and even severe, persistent bullying.
Who is Most at Risk?
Certain factors increase vulnerability to complex post traumatic stress disorder:
- Childhood trauma exposure: This is the highest risk factor because it occurs while the brain is still developing. This can lead to what is sometimes called Developmental Trauma Disorder (DTD).
- Lack of social support: Isolation during or after trauma is profoundly damaging, especially when the abuser was supposed to be a protector.
- Pre-existing mental health conditions: Conditions like anxiety or depression can make it harder to cope with chronic trauma.
- Systemic oppression and racism: Continuous exposure to discrimination and prejudice creates a form of “continuous traumatic stress” that erodes one’s sense of safety.

Complex PTSD in Children and Adolescents
When C-PTSD develops in childhood, it impacts every aspect of growth. When caregivers are a source of trauma instead of security, it creates a developmental crisis.
- Impact on development: Chronic trauma disrupts brain areas responsible for emotional regulation, executive function, and memory.
- Attachment issues: Children may develop “disorganized attachment,” simultaneously wanting and fearing closeness.
- Behavioral problems: Aggression, defiance, withdrawal, or self-harm can be attempts to cope with internal distress.
- Learning difficulties: A constantly activated alarm system makes it hard to focus, learn, and remember information at school.
- Emotional regulation challenges: Explosive outbursts or emotional numbness reflect a nervous system that hasn’t learned to find balance.
Early recognition and intervention are critical. Our specialized programs understand these unique developmental needs and provide age-appropriate support. For details about care custom to this age group, see our programs for young adults, which outline treatment options designed specifically for this population.
Pathways to Healing: Evidence-Based Treatments for Complex Post Traumatic Stress Disorder
If you’re in crisis, call or text 988 right now. Help is available 24/7.
Healing from complex post traumatic stress disorder is absolutely possible. While recovery isn’t a straight line, thousands have rebuilt fulfilling lives. Effective treatment often follows a phased approach developed by trauma pioneer Judith Herman.
- Phase 1: Safety and Stabilization. The first step is learning to feel safe in your own body. This involves developing skills to manage overwhelming emotions and ground yourself during dissociation.
- Phase 2: Trauma Processing and Remembrance. Once you have stabilization skills, you can work with a therapist to carefully process traumatic memories, reducing their emotional charge so they no longer hijack your daily life.
- Phase 3: Integration and Reconnection. This phase focuses on building the life you want by developing a positive relationship with yourself, improving connections with others, and finding new meaning.

Therapies That Work for CPTSD
Several evidence-based therapies are effective for complex post traumatic stress disorder. The key is finding the right fit with a therapist who understands complex trauma.
- Skills Training in Affective and Interpersonal Regulation (STAIR): Teaches practical skills for managing intense emotions and building healthier relationships.
- Eye Movement Desensitization and Reprocessing (EMDR): Uses bilateral stimulation (like eye movements) to help the brain process traumatic memories and reduce their emotional intensity. We offer Eye Movement Desensitization and Reprocessing (EMDR) as part of our comprehensive care.
- Dialectical Behavior Therapy (DBT): Highly effective for C-PTSD, DBT teaches skills in mindfulness, distress tolerance, emotion regulation, and interpersonal effectiveness. Learn more about our Dialectical Behavior Therapy Components.
- Cognitive Behavioral Therapy (CBT): Trauma-focused CBT helps identify and change unhelpful thought patterns that developed as survival mechanisms. We offer Online Cognitive Therapy.
- Somatic Experiencing: A body-based approach that helps release trauma “stuck” in the nervous system by focusing on physical sensations.
- Internal Family Systems (IFS): Views the psyche as having different “parts” and helps you heal them to foster self-compassion and internal harmony.
Medication, such as antidepressants, can also be helpful for managing symptoms like depression or anxiety during therapy. Our Intensive Outpatient Programs and Virtual Intensive Outpatient Programs integrate these therapies into personalized treatment plans.
Managing Symptoms and Improving Quality of Life
Beyond therapy, these strategies can improve your daily life with complex post traumatic stress disorder:
- Grounding techniques: Use the 5-4-3-2-1 method (name 5 things you see, 4 you touch, etc.) to return to the present during flashbacks or dissociation.
- Mindfulness practices: Observe your thoughts and feelings without judgment to reduce reactivity.
- Journaling: A safe space to process emotions and identify patterns or triggers.
- Building a support system: Start small by connecting with a trusted friend, family member, or a trauma support group.
- Self-compassion: Treat yourself with the same kindness you would offer a friend.
- Healthy lifestyle choices: Regular exercise, balanced nutrition, and consistent sleep significantly impact mood and energy.
- Creative outlets: Use art, music, or writing to express emotions that are hard to put into words. Read more about the healing power of art.
You can read more about trauma-informed care on our blog for additional strategies and insights.
Insurance and Access to Care
We know finding quality care for complex post traumatic stress disorder is overwhelming. We are in-network with major insurers like Cigna, Optum, and Florida Blue to reduce out-of-pocket costs. Our virtual and hybrid intensive outpatient (IOP) and partial hospitalization (PHP) programs offer flexible scheduling, including evening options.
Whether you’re in Tampa Bay, St. Petersburg, Miami, Orlando, or anywhere else in Florida, our telehealth services bring expert care to your home.
You can find more info about our partial hospitalization (PHP) programs and learn how we work with various insurance providers to make treatment accessible. Recovery from complex post traumatic stress disorder is a journey, but you don’t have to walk it alone.
Frequently Asked Questions about Complex PTSD
SUGGESTION: Implement JSON-LD FAQPage schema markup for this section.
Here are answers to common questions about complex post traumatic stress disorder.
Can you have both PTSD and C-PTSD?
Yes, but if you meet the criteria for both, the ICD-11 recommends a C-PTSD diagnosis. This is because C-PTSD provides a more complete picture, encompassing the core PTSD symptoms plus the additional difficulties with emotional regulation, self-worth, and relationships. This guides a more comprehensive treatment plan.
Is C-PTSD a lifelong condition?
No, C-PTSD is not a life sentence. With appropriate, long-term, trauma-informed treatment, significant healing is possible. While some sensitivities may remain, you can learn to manage symptoms, build healthy relationships, and live a fulfilling life. The trauma becomes part of your story, but it doesn’t have to be the whole story.
How do I support a loved one with C-PTSD?
Supporting someone with complex post traumatic stress disorder can make a huge difference in their recovery. Here are a few key ways to help:
- Educate yourself: Learn about C-PTSD to understand their symptoms and respond with compassion instead of frustration.
- Be patient: Healing takes time and has ups and downs. Your consistent, non-judgmental support provides a sense of safety.
- Encourage professional help: Gently suggest therapy but respect their autonomy. The decision to seek help must be theirs.
- Create stability: Maintain routines and be reliable. A predictable environment can be incredibly healing for someone whose world felt chaotic.
- Practice self-care: Supporting a loved one is demanding. Ensure you have your own support system to avoid burnout.
Take the First Step Toward Healing
Recovery from complex post traumatic stress disorder is a journey toward understanding, healing, and reclaiming your life. The fact that you’re reading this shows incredible courage and is an important first step.
Understanding C-PTSD is powerful. It helps you make sense of experiences that may have felt confusing for years, reframing them not as character flaws but as normal responses to abnormal situations.
You don’t have to face this alone. At Thrive Mental Health, we understand the unique challenges of complex trauma. Our virtual and hybrid intensive outpatient (IOP) and partial hospitalization (PHP) programs offer flexible evening options, making it easier to prioritize your healing.
Our expert-led approach combines therapies like EMDR, DBT, and trauma-focused CBT in a supportive environment. Our telehealth services bring quality care to you, with a special focus on serving communities across Florida.
Getting started is simple and confidential. You can verify your insurance coverage in just 2 minutes (no obligation), or call us directly at 561-203-6085 to speak with someone who understands. We work with major insurers like Cigna, Optum, and Florida Blue to help make treatment accessible.
If you’re in crisis right now, please call or text 988. Help is available 24/7, and you deserve support.
Healing from complex post traumatic stress disorder takes time, but it is absolutely possible. With the right support, you can learn to manage symptoms, build healthier relationships, and create a life that feels genuinely yours. Your journey toward healing can begin today.