Active vs Passive Suicidal Thoughts Survival Guide

Active vs Passive Suicidal Thoughts: Get Urgent Help 2025
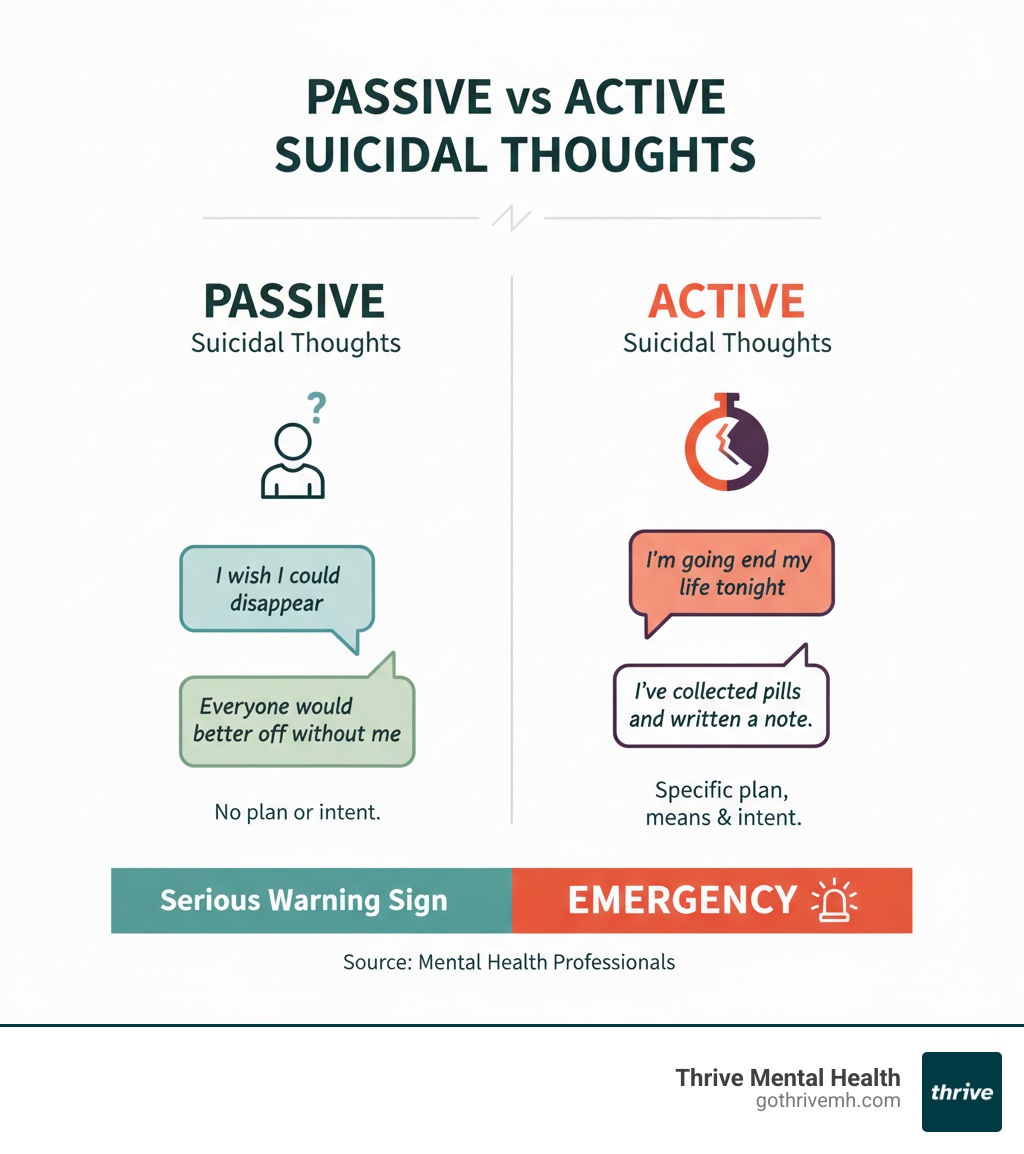
Passive vs Active Suicidal Thoughts: What’s the Real Difference?
What’s the difference between active vs passive suicidal thoughts and where can I find help? Here’s what you need to know right now:
Quick Answer:
- Passive suicidal thoughts = Wishing you were dead, but no plan to act. Example: “I wish I wouldn’t wake up.”
- Active suicidal thoughts = Having a specific plan, intent, or means to end your life. Example: “I’m going to take these pills tonight.”
- Where to get help: Call 988 (Suicide & Crisis Lifeline) immediately if you or someone you know has active suicidal thoughts. For passive thoughts, contact a mental health professional right away.
If you’re in crisis, call or text 988 right now. You are not alone.
Ignoring suicidal thoughts—passive or active—can cost lives. But acting now can save yours or someone you love. The difference between passive and active suicidal ideation isn’t just clinical language. It’s the difference between a warning sign and an emergency. It’s the difference between “I need help soon” and “I need help right now.”
This guide will teach you how to spot the difference, what warning signs demand immediate action, and where to find fast, effective treatment.
The landscape of suicidal ideation is complex. The main distinction between passive and active suicidal ideation lies in the presence of intent and a plan. Understanding this is essential for assessing risk and determining the right level of intervention.
What is Passive Suicidal Ideation?
Passive suicidal ideation involves thoughts about death or a wish to be dead, but without a specific plan or intent to act. It’s a profound sense of hopelessness, often manifesting as a wish to “disappear” or “not wake up.” Examples include:
- “I wish I was never born.”
- “They’d all be better off without me.”
- “I don’t want to live anymore.”
- “I wish I could go to sleep and never wake up.”
While there’s no immediate plan, passive suicidal ideation is a serious indicator of distress. It signifies a deep emotional struggle that, if left unaddressed, can escalate into active ideation.
What is Active Suicidal Ideation?
Active suicidal ideation is characterized by thoughts of self-harm that include a plan, means, and clear intent. This is a critical stage where the person has moved from wishing for death to actively preparing for it. Signs include:
- “It would be so easy to end my life by [specific method].”
- “I should write a goodbye note.”
- “I have a plan in place.”
- “I am going to kill myself.”
Sometimes, a person may appear suddenly calm, as if a decision has been made. This can be an alarming sign mistaken for improvement. Active suicidal ideation requires emergency treatment due to the immediate risk.
Why the Distinction Matters
The distinction between passive and active ideation is about understanding the level of immediate risk to guide the response. Openly discussing suicide provides a better chance to help. While passive thoughts seem less urgent, they are a cry for help and a significant risk factor for future active ideation. Both forms demand professional intervention.
[TABLE] Passive vs Active Suicidal Thoughts: Key Differences
| Feature | Passive Suicidal Thoughts | Active Suicidal Thoughts |
|---|---|---|
| Intent to Die | No | Yes |
| Suicide Plan | No | Yes |
| Access to Means | No | Often Yes |
| Immediacy of Risk | Lower (but real) | High—needs urgent help |
How to Spot the Signs—And What to Do Next

Recognizing suicidal ideation isn’t always easy. People in pain often hide it behind forced smiles and texts saying, “I’m fine.” But there are signs, and knowing them can save a life.
Signs of Passive Suicidal Ideation
Passive thoughts come with quiet warning signs that someone is struggling.
- Expressions of hopelessness: Phrases like “What’s the point?” or “Nothing will ever get better.”
- Feeling like a burden: Saying things like, “People would be better off without me.”
- Social withdrawal: Suddenly canceling plans or becoming distant and isolated.
- Dramatic changes in sleep: Sleeping excessively to escape or barely sleeping at all due to intrusive thoughts.
- Increased risky behavior: Reckless driving or excessive drinking that shows a disregard for personal safety.
- Giving away valued possessions: Insisting you take a favorite item without a clear reason.
Research on childhood trauma shows that past trauma significantly increases this risk. If someone has a history of abuse, these signs are even more critical.
Signs of Active Suicidal Ideation
Active suicidal thoughts are an emergency. The signs are more direct and require immediate intervention.
- Explicit talk about suicide: Statements like “I’m going to kill myself” or “I wish I were dead.” Believe them. This is a crisis.
- Developing a specific plan: Talking about how, when, or where they intend to end their life.
- Actively seeking means: Acquiring weapons, stockpiling pills, or researching lethal methods.
- Making final arrangements: Writing a will, distributing possessions, or updating life insurance.
- Saying final goodbyes: Visiting or calling loved ones with an unusual sense of closure.
- Sudden calm after severe depression: An unexpected sense of peace can mean they’ve decided to end their life and feel relief that the pain will soon be over.
Key Risk Factors for Suicidal Ideation
Understanding what’s the difference between active vs passive suicidal thoughts and where can I find help means recognizing who’s most vulnerable.
- Mental health conditions: Depression, anxiety, bipolar disorder, and PTSD significantly increase risk, especially when untreated.
- Trauma history: Childhood abuse, neglect, or other traumas create lasting wounds.
- Substance use: Alcohol and drugs impair judgment and increase impulsivity.
- Major life stressors: Job loss, divorce, financial collapse, or the death of a loved one can be triggers.
- Lack of support: Isolation and loneliness intensify hopelessness. A 2022 report found 45% of LGBTQIA+ youth seriously considered suicide, often due to unsupportive environments.
- Chronic illness or pain: Persistent physical suffering can lead to a feeling that death is the only escape.
- Family history: A family history of suicide can indicate genetic predisposition and learned coping patterns.
Remember: Any thought of suicide is serious. It’s always best to err on the side of caution. If someone expresses thoughts of not wanting to be alive, they need evaluation by a mental health provider. You don’t need to diagnose—just recognize the signs and help them connect to care.
What to Do If You or Someone You Love Has Suicidal Thoughts
When someone is struggling with suicidal thoughts, knowing what to do can save a life. The right response depends on the immediacy of the risk, but every suicidal thought must be taken seriously. Never assume it’s an overreaction; the worst thing you can do is nothing.
Emergency Steps for Active Suicidal Thoughts
If someone has active suicidal thoughts with a plan and intent, it’s a mental health emergency. Act now.
- Call 988 or 911 immediately. The 988 Suicide & Crisis Lifeline provides 24/7 access to trained counselors. If the danger is immediate, call 911.
- Do not leave the person alone. Stay with them until professional help arrives. Your presence is a crucial safety buffer.
- Remove access to means. Secure or remove firearms, medications, sharp objects, or anything else that could be used for self-harm.
- Go to the nearest emergency room. The ER is equipped to handle psychiatric emergencies and can provide immediate stabilization.
- Listen without judgment. Ask directly: “Are you thinking about hurting yourself right now?” Asking does not plant the idea; it shows you’re willing to face the truth with them.
For more guidance, our Crisis Mental Health Emergency Services resource offers detailed support.
Urgent Steps for Passive Suicidal Thoughts
Passive suicidal thoughts are a flashing red light demanding action. Think of them as smoke before a fire.
- Contact a mental health professional ASAP. Schedule an appointment with a therapist or psychiatrist for a thorough assessment.
- Tell a trusted friend or family member. Isolation amplifies suicidal thoughts. Sharing what you’re going through is a lifeline.
- Make a safety plan. This is a fire escape route for your mental health, outlining triggers, coping strategies, and contacts. Work with a professional to create one.
- Remove potential harm items. Even with passive thoughts, limiting access to means is a simple, effective precaution.
- Schedule and attend therapy. Consistent professional support, whether in-person or virtual, is one of the most effective ways to address suicidal ideation. Our Online Therapy programs make it easy to access care.
How Loved Ones Can Help
Supporting someone with suicidal thoughts can feel overwhelming. Here’s what actually helps:
- Ask the direct question: “Are you thinking about suicide?” Research shows this can decrease suicidal ideation.
- Listen without fixing. You don’t need answers. Just sit with them in their pain and validate their feelings. Say, “I’m here, and I’m not going anywhere.”
- Express concern and offer concrete support. Tell them they matter and help them research therapists or make appointments.
- Help connect them to professional care. Be the bridge to the help they need. Our Mental Health Crisis Guide offers guidance for loved ones.
- Set boundaries to protect yourself. Supporting someone in crisis is exhausting. You need your own support system. Taking care of yourself isn’t selfish—it’s essential.
Real Treatment, Real Recovery: What Works for Suicidal Thoughts
Recovery from suicidal ideation isn’t just possible—it’s happening every day. It’s about getting the right, evidence-based treatment from professionals who know what they’re doing. At Thrive Mental Health, we’ve seen thousands move from their darkest moments to sustainable recovery.
Evidence-Based Care: Therapies That Transform
When you need help, you need to know what actually works. These therapies save lives.
- Cognitive Behavioral Therapy (CBT): This highly effective treatment teaches you to identify, challenge, and replace the negative thought patterns that fuel suicidal thinking with practical coping skills.
- Dialectical Behavior Therapy (DBT): DBT is especially powerful for those with intense emotions or a history of self-harm. It teaches core skills in mindfulness, distress tolerance, emotion regulation, and interpersonal effectiveness.
- Group and Family Therapy: Group therapy breaks the cycle of isolation by connecting you with others who understand. Family therapy brings your support system into the healing process, improving communication and accelerating recovery.
- Medication Management: Antidepressants or mood stabilizers can balance brain chemistry, making therapy more effective by lifting depression enough to practice new skills. A psychiatrist can determine if medication is right for you.
Levels of Care at Thrive Mental Health
We offer different programs to meet you exactly where you are.
- Intensive Outpatient Programs (IOP): Get serious clinical support (3-4 hours a day, several days a week) while maintaining your daily life. Our Intensive Outpatient Programs combine individual therapy, group sessions, and psychiatric care.
- Partial Hospitalization Programs (PHP): This is a higher level of care (5-6 hours a day, 5 days a week) that provides hospital-level treatment without the hospital stay. It’s an ideal step-down from inpatient care or step-up from IOP.
Our programs are built for real life, with virtual and hybrid options, including evening programs and telehealth sessions. Our Virtual Therapy options offer flexible, effective care without the commute.
Accessible Care in Your Community
We serve communities across Florida, including Tampa Bay, St. Petersburg, Miami, Orlando, Boca Raton, West Palm Beach, Jacksonville, Fort Lauderdale, Naples, and Sarasota.
We accept most major insurance plans, including Cigna, Optum, and Florida Blue. Cost shouldn’t be a barrier to life-saving treatment. Verify your insurance in two minutes with zero obligation.
FAQs: Active vs Passive Suicidal Thoughts
You’re not alone if you have questions about what’s the difference between active vs passive suicidal thoughts and where can I find help. Here are clear, honest answers to common concerns.
Can passive suicidal thoughts turn active?
Yes, and it can happen quickly. A crisis, major stressor, or loss can cause passive thoughts to escalate into active plans within minutes. That’s why all suicidal thoughts must be taken seriously. Early intervention is key to preventing escalation.
Is it safe to ask someone if they’re thinking about suicide?
Absolutely. Research proves that asking directly does NOT increase risk—it can actually decrease it. When you ask, “Are you thinking about suicide?” you open a door for them to get help and show them you are not afraid of their pain. It can be a life-saving conversation.
What’s the difference between suicidal thoughts and intrusive thoughts?
Suicidal thoughts involve a genuine wish to die, whether passive or active. Intrusive thoughts are unwanted, distressing ideas that pop into your head and don’t reflect your true desires. A mental health professional can help you distinguish between them, but either way, you deserve support.
Does insurance cover treatment for suicidal thoughts?
Yes, most major insurance plans cover evidence-based treatment for suicidal ideation, including therapy, IOP, and PHP programs. Plans like Cigna, Optum, and Florida Blue typically cover the intensive care that leads to recovery. Coverage details vary, so we make it easy to find out what your benefits include. You can verify your insurance here in about two minutes—no obligation.
Where can I get help in Florida?
Thrive Mental Health offers virtual and hybrid IOP/PHP programs across Florida. You can access expert-led treatment from home or at one of our centers. Our programs include evening options and flexible scheduling. See locations and program options on our website to get started.
Summary: Don’t Wait—Get Help for Suicidal Thoughts Now
You now know the critical answer to what’s the difference between active vs passive suicidal thoughts and where can I find help? Active thoughts include a plan and intent, requiring an emergency response. Passive thoughts are wishes to be dead without a plan, but are still a serious warning sign. The most important takeaway is that both are serious and treatable. Recovery is not just possible; it’s expected with the right support. Thrive Mental Health provides that support through flexible virtual and hybrid IOP/PHP programs covered by most major insurance (including Cigna, Optum, and Florida Blue) in Florida. Don’t wait for thoughts to escalate. For next steps, learn How to Make a Safety Plan for Suicidal Thoughts and take action today.
Ready for Support? Take the First Step Now
You’ve made it this far. That means something. It means you’re looking for answers, for hope, for a way forward. And that takes courage.
If you or someone you love is struggling with suicidal thoughts—passive or active—you don’t have to steer this alone. Thrive Mental Health is here to help, right now, wherever you are.
We offer virtual and hybrid IOP and PHP programs designed for real life. That means flexible scheduling, including evening options that work around your job, your family, your responsibilities. We combine expert clinical care with the convenience of telehealth and the support of in-person centers across Florida.
Our programs are covered by most major insurance plans—including Cigna, Optum, Florida Blue, and more. You can verify your benefits in about two minutes, with no obligation and no pressure. Just clarity on what’s covered and what your next step could be.
Ready to start? Verify your insurance here. Our team will walk you through your options, answer your questions, and help you take that first step toward real recovery.
If you’re in crisis right now, don’t wait. Call or text 988. The National Suicide & Crisis Lifeline is available 24/7, and trained counselors are standing by to help. You are not alone. You are worth saving. And help is always, always within reach.