What Does Dialectical Mean in Dialectical Behavior Therapy? Solving the DBT Puzzle

What does dialectical mean in dialectical behavior therapy!
That Confusing “D” in DBT
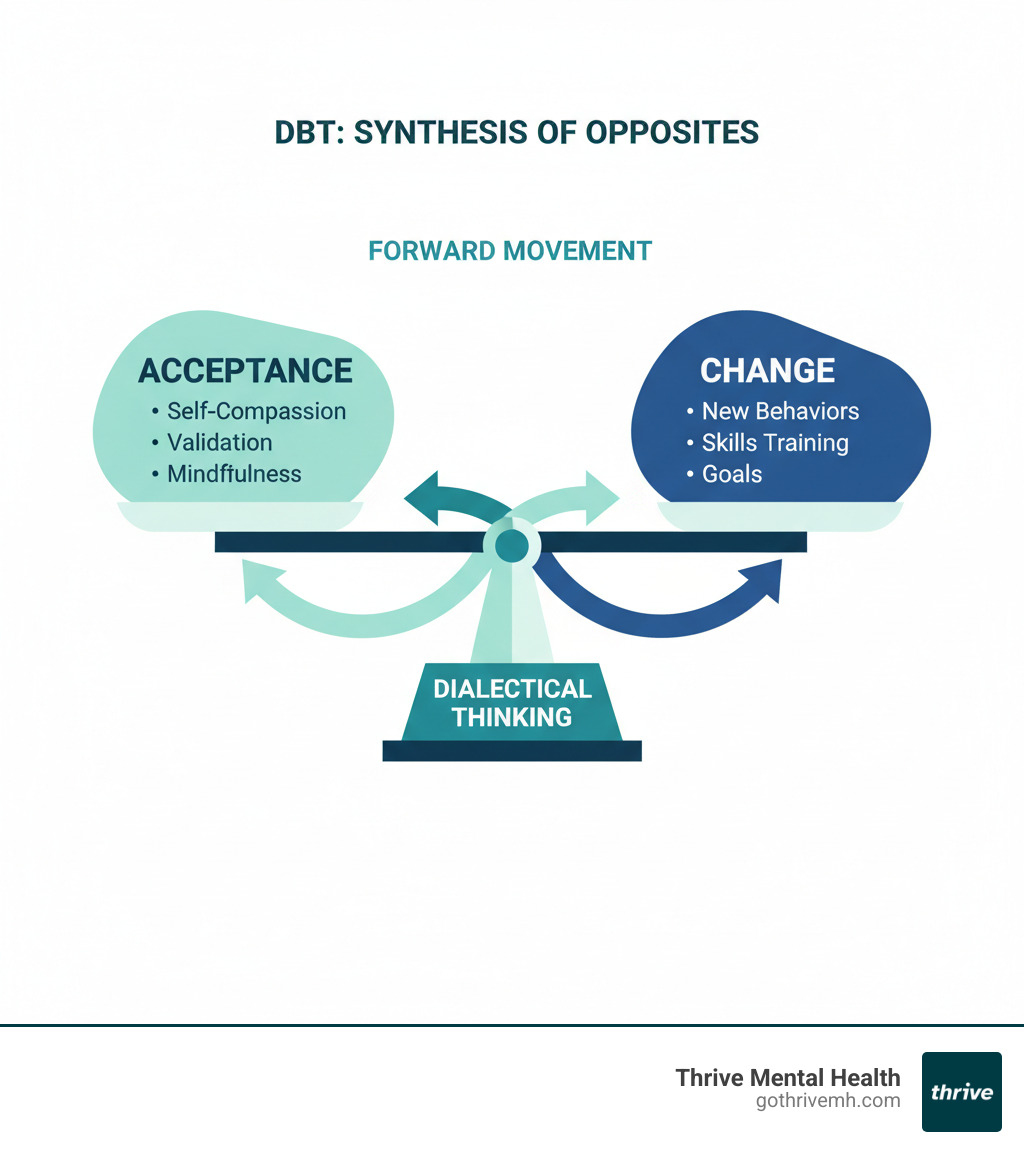
What does dialectical mean in dialectical behavior therapy? In DBT, dialectical means recognizing that two seemingly opposite things can both be true at the same time. It’s the core principle of balancing acceptance of yourself and your current reality with the need to make positive changes—holding both truths together using “and” instead of “but.”
Quick Answer:
- Dialectical = synthesis of opposites
- In DBT, it means: Acceptance AND Change
- You can accept yourself as you are AND work to do better
- It helps you move beyond black-and-white, all-or-nothing thinking
- The word comes from philosopher Georg Hegel’s work on integrating opposing ideas
Most people have never heard the word “dialectical” before learning about DBT. When you’re struggling with intense emotions, depression, or trauma, the last thing you need is confusing therapy jargon. You just want to know if this treatment will actually help.
Here’s the truth: understanding what “dialectical” means open ups why DBT works when other therapies haven’t. It’s not about choosing between accepting your pain or changing your life. It’s about doing both at once.
As Nate Raine, CEO of Thrive Mental Health, I’ve seen how grasping this core concept helps clients break free from emotional extremes and build lives they actually want to live. My work scaling evidence-based behavioral health programs across Florida has shown me that what does dialectical mean in dialectical behavior therapy is often the most important question someone asks before committing to treatment.
What does dialectical mean in dialectical behavior therapy terms simplified:
- dialectical behavior therapy components
- how does dialectical behavioral therapy work
- what does dialectical behavior therapy treat
The Core of ‘Dialectical’: How Two Opposing Truths Create a Path Forward
At its heart, “dialectical” signifies the “existence of opposites” or “the synthesis or integration of opposites.” It’s the profound idea that two seemingly contradictory ideas or feelings can coexist and even inform each other. Marsha Linehan, the visionary behind DBT, emphasizes that there’s often a “kernel of truth” in opposing ideas. This might sound confusing at first, but it’s a powerful shift from the rigid, all-or-nothing thinking that often fuels emotional distress.
Instead of viewing the world in stark “black or white” terms, dialectical thinking encourages us to accept the “gray” – the nuances and complexities of life. It helps us move beyond the harmful trap of an “all-or-nothing mindset” where we feel we must choose one extreme over another. For example, rather than thinking “I am a complete failure because I made a mistake,” dialectical thinking allows for “I made a mistake, AND I am still a capable person.”
This concept isn’t new; its roots stretch back to ancient philosophy. The German philosopher Georg Hegel, in the 1800s, famously established the “thesis—antithesis—synthesis” model of logic. He proposed that an idea (thesis) would inevitably encounter an opposing idea (antithesis), and through their conflict, a new, more comprehensive idea (synthesis) would emerge. This philosophical foundation underpins DBT’s approach to integrating seemingly contradictory concepts like acceptance and change. It’s about finding a “middle path” that isn’t necessarily a compromise, but a richer, more effective way forward.
The Power of “And” Over “But”
Here’s where what does dialectical mean in dialectical behavior therapy gets practical: it’s about changing one tiny word that makes a massive difference in how you feel about yourself.
Think about the difference between these two sentences: “I love you, but I’m angry with you” versus “I love you, and I’m angry with you.” Feel that shift? When you use “but,” you’re basically erasing everything that came before it. The love suddenly feels fake or conditional. It’s like you’re saying “ignore that first part—here’s what I really mean.”
But when you use “and,” both things get to be true at the same time. The love is real. The anger is real. Neither one cancels out the other. This isn’t just grammar—it’s a complete shift in how we validate our own experiences and emotions.
This simple word swap becomes a powerful tool for shifting your internal dialogue. Instead of beating yourself up with “I’m trying hard, but I keep failing,” you can say “I’m trying hard, and I’m still learning.” See how the second version doesn’t throw out your effort? It acknowledges where you are while leaving room for growth.
Using “and” helps you reduce self-judgment in ways that feel almost magical once you get the hang of it. When you can hold two truths at once—like “I made a mistake and I’m still a good person”—you stop living in that exhausting world where one slip-up means total failure. You’re fostering self-compassion by allowing yourself to be human: flawed, growing, worthy, and imperfect all at once.
This is what therapists mean when they talk about validation. You’re not dismissing your struggles with toxic positivity. You’re not wallowing in self-criticism either. You’re simply acknowledging reality in all its messy complexity.
Common Dialectics You Experience Every Day
Once you start looking for dialectics, you’ll see them everywhere. These “both/and” truths show up constantly in real life, even when we don’t have fancy words for them.
“I am doing the best I can AND I need to do better” might be the most important dialectic in DBT. It’s the foundation of the whole approach—honoring your current efforts while still pushing toward growth. No shame, no excuses, just honest acknowledgment of where you are and where you’re headed.
“I accept myself for who I am AND I want to change” captures what trips up so many people in therapy. They think accepting themselves means giving up on growth, or that wanting to change means rejecting who they are now. Neither is true. You can hold both.
“This is painful AND I can get through this” is the dialectic that gets people through crisis moments. You’re not pretending it doesn’t hurt. You’re not drowning in hopelessness. You’re acknowledging the pain while trusting your ability to survive it.
“I am scared AND I am brave enough to face this” reminds us that courage isn’t the absence of fear—it’s feeling the fear and moving forward anyway. You don’t have to wait until you’re not scared. You can be both terrified and capable at the exact same time.
These dialectics aren’t just therapy exercises. They’re how life actually works. Your family can frustrate you and you can love them deeply. Life can be beautiful and brutal (some people call it “brutaful”). You can have a diagnosis like Borderline Personality Disorder and be so much more than that label.
When you start thinking this way, you stop getting stuck in impossible either-or choices. You find that middle path where real change actually happens.
What Does Dialectical Mean in Dialectical Behavior Therapy in Practice?
So, what does dialectical mean in dialectical behavior therapy when you’re actually sitting in a session or practicing skills at home? It all comes down to one fundamental truth: Acceptance AND Change aren’t opposites—they’re partners.
This is the beating heart of DBT. It’s not a side note or a nice idea. It’s the foundation everything else is built on.
Here’s what most people don’t understand until they experience it: you can’t change something you’re fighting against. If you’re constantly at war with yourself—hating your emotions, judging your reactions, refusing to acknowledge your pain—you stay stuck. Real, lasting change only happens when you first accept where you are right now.
Let’s say you’re struggling with self-harm. Traditional therapy might focus solely on stopping the behavior. DBT does something different. It starts by validating the intense emotional pain that drives you to self-harm in the first place. Your therapist will acknowledge that your pain is real, that it makes sense given your history, and that you’ve been doing your best to survive. That’s the acceptance piece.
And at the same time, DBT teaches you new, healthier ways to cope with that pain. Skills to tolerate distress without making it worse. Ways to regulate your emotions before they become overwhelming. That’s the change piece.
Both happen together. Not one after the other. Not one instead of the other. Both, at the exact same time.
This is what therapists mean when they talk about “holding the dialectic.” They’re constantly balancing validation (“I understand why you feel this way, and your feelings are valid”) with gentle pushes toward change (“And now, let’s explore a skill that could help you respond differently next time”). It’s a delicate dance, and when done well, it keeps you from getting stuck in emotional extremes or rigid thinking patterns.
The ultimate goal? Creating what DBT calls a “life worth living”—a life that feels meaningful, connected, and genuinely worth getting up for. Not a life free of pain (that’s not realistic), but a life where you have the skills to handle pain without it destroying everything else. Dialectical Behavior Therapy (DBT) provides the structured, evidence-based roadmap to get there.
How DBT Differs from Traditional CBT
DBT grew out of Cognitive Behavioral Therapy (CBT), but it’s not just “CBT with extra steps.” Understanding the differences helps clarify why what does dialectical mean in dialectical behavior therapy matters so much—and why DBT might be the right fit when other therapies haven’t worked.
CBT focuses primarily on changing your thoughts to change your feelings and behaviors. The core idea is that distorted thinking patterns drive emotional distress, so if you can identify and restructure those thoughts, you’ll feel better. It’s incredibly effective for many people, especially those dealing with anxiety and depression.
DBT takes a different approach. It starts with the assumption that your emotions are valid responses to your experiences—even the intense, overwhelming ones. The problem isn’t necessarily your thoughts (though those matter too). The problem is that you haven’t learned effective ways to regulate and tolerate intense emotions. DBT emphasizes acceptance of your emotional reality first, then teaches change skills.
Here’s how they compare in practice:
| Feature | Dialectical Behavior Therapy (DBT) | Cognitive Behavioral Therapy (CBT) |
|---|---|---|
| Primary Focus | Emotions and acceptance | Thoughts and cognitive patterns |
| Core Principle | Dialectics (both/and thinking) | Cognitive restructuring (challenging distorted thoughts) |
| Best For | Intense emotional dysregulation, BPD, chronic suicidal ideation, self-harm | Anxiety, depression, phobias, PTSD |
| Treatment Structure | Individual therapy, skills training groups, phone coaching, therapist consultation team | Typically individual sessions with homework assignments |
One key difference: DBT was specifically designed for people who experience emotions very intensely—so that traditional talk therapy alone often isn’t enough. If you’ve tried CBT and found yourself thinking “I understand what you’re saying, but I can’t do it when I’m this upset,” that’s exactly the gap DBT fills. It gives you concrete skills to use in the moment when your emotions feel like they’re going to swallow you whole.
The research backs this up. DBT has been proven to significantly decrease suicide-related outcomes, psychiatric hospitalizations, emergency room visits, and treatment dropout rates. It reduces depression and substance use while increasing social functioning. These aren’t small improvements—they’re life-changing shifts.
Who Benefits from a Dialectical Approach?
The dialectical approach in DBT is especially powerful for people who feel emotions at a volume most others can’t imagine. If your emotional reactions feel like they go from 0 to 100 in seconds, if small disappointments can spiral into crises, if you’ve been told you’re “too sensitive” or “too much”—DBT was designed with you in mind.
Marsha Linehan originally developed DBT for people with Borderline Personality Disorder (BPD), particularly those struggling with chronic suicidal thoughts and self-harm. For this population, DBT remains the gold standard treatment, helping manage the extreme mood swings, impulsive behaviors, and intense fear of abandonment that characterize BPD.
But here’s what’s remarkable: the skills work for so many other conditions where emotional dysregulation plays a central role. DBT has proven effective for people dealing with chronic suicidal ideation and self-harm behaviors, even when BPD isn’t the primary diagnosis. It provides critical, life-saving skills to manage overwhelming urges and build reasons for living.
People with Post-Traumatic Stress Disorder (PTSD) benefit from DBT’s emphasis on distress tolerance and emotion regulation, learning to manage the intense emotional flashbacks and hyperarousal that trauma creates. Those struggling with eating disorders—particularly bulimia and binge-eating disorder—find that DBT addresses the emotional dysregulation and impulsivity underlying their behaviors.
For substance use disorders, DBT offers healthier coping mechanisms to replace the numbing or escape that drugs and alcohol provide. And for people with severe or treatment-resistant depression and anxiety, DBT fills in the gaps when symptom management alone isn’t enough.
The common thread? All of these conditions involve difficulty managing intense emotions in healthy ways. That’s where the dialectical approach shines—accepting the intensity of what you’re feeling while building new skills to respond differently.
For many people with these conditions, once-a-week therapy simply isn’t enough structure or support. That’s where virtual IOP programs come in. At Thrive Mental Health, we provide intensive DBT programming across Florida—designed for people who need more than weekly sessions but less than inpatient care. Our programs combine expert clinical care with the flexibility of virtual treatment and evening scheduling options.
Most major insurance plans, including Cigna, Optum, and Florida Blue, cover DBT as part of IOP or PHP programs. Verify your insurance benefits in 2 minutes to see what’s covered under your specific plan—no obligation, just information.
If you’re in crisis, call/text 988 right now. You are not alone. The National Suicide Prevention Lifeline is available 24/7 with trained counselors who understand what you’re going through.
How DBT’s 4 Core Skills Put Dialectics into Action

So what does dialectical mean in dialectical behavior therapy when you’re actually sitting in a session or practicing skills at home? It means learning four specific skill sets that perfectly balance acceptance and change. These aren’t abstract concepts—they’re practical tools you can use today, tonight, or the next time you’re in crisis.
Think of these four skill modules as your emotional survival kit. Two focus on acceptance (meeting yourself where you are), and two focus on change (building the life you want). Together, they create measurable improvements in emotional stability, relationship quality, and overall well-being.
Here’s how they work in real life: Imagine you’re learning to ride a bike. You need to accept that balance is hard at first (acceptance) and keep pedaling forward anyway (change). Stop pedaling, and you fall. Fight the wobbling, and you crash. DBT teaches you to do both at once.
Acceptance Skills: Finding Your Footing in the Storm
When emotions hit like a hurricane, acceptance skills help you stand firm without getting swept away. These aren’t about giving up or resigning yourself to suffering—they’re about acknowledging reality so you can work with it instead of against it.
Mindfulness is the foundation of everything in DBT. It teaches you to be present in this exact moment, observing your thoughts and feelings without drowning in them or judging yourself for having them. This is where radical acceptance comes in—the practice of fully accepting reality as it is, even when it’s painful, because fighting reality only creates more suffering. When you’re mindful, you notice the “kernel of truth” in your experience without letting it define you. You see the thought “I’m worthless” as just a thought, not a fact. Most DBT programs teach mindfulness first because every other skill builds on this foundation.
Distress Tolerance is your crisis survival toolkit. Sometimes life throws situations at you that can’t be fixed in the moment—a loss, a rejection, an overwhelming urge to hurt yourself. These skills teach you how to survive crises without making them worse. You learn self-soothing techniques, healthy distractions, and ways to handle emotional pain that don’t involve behaviors you’ll regret later. The goal isn’t to feel good—it’s to get through the storm without capsizing your boat. You ride the wave instead of being crushed by it.
Change Skills: Building a New Way Forward
Once you’ve found your footing and learned to weather the storm, you’re ready to build something new. Change skills give you the power to reshape your emotional life and relationships into what you actually want them to be.
Emotion Regulation teaches you to understand and manage your emotions instead of being controlled by them. You learn to identify what you’re feeling, understand why it’s happening, and reduce your vulnerability to emotional meltdowns. Skills like “checking the facts” help you see if your emotional reaction matches reality, while “opposite action” teaches you to act against unhelpful emotion urges. You also learn practical ways to reduce emotional vulnerability—getting enough sleep, eating regularly, exercising—because it’s hard to regulate emotions when your body is running on empty. This module is about becoming the master of your emotions, not their prisoner.
Interpersonal Effectiveness focuses on relationships, which are often both our greatest source of joy and our biggest trigger for pain. These skills teach you how to ask for what you need without feeling guilty, say no without destroying relationships, and maintain your self-respect while still connecting with others. It’s the dialectic of prioritizing your needs and maintaining relationships, getting what you want and keeping the other person. For many people in our Florida-based virtual IOP programs, these skills transform their most important relationships within weeks.
Together, these four modules give you a complete toolbox for building a life worth living. Research shows that people who complete DBT see significant decreases in suicidal behavior, self-harm, psychiatric hospitalizations, and substance use, while experiencing major improvements in their ability to function day-to-day. The skills work—if you practice them.
Frequently Asked Questions about the Dialectical Approach in DBT
What is the main goal of DBT?
When people ask me what DBT is really trying to accomplish, I tell them: it’s about building a life worth living. Not just surviving. Not just getting through the day. Actually living in a way that feels meaningful and manageable.
What does dialectical mean in dialectical behavior therapy in practical terms? It means learning skills to manage intense emotions, reduce self-destructive behaviors, and improve relationships—all while holding that central balance between accepting yourself and changing what you can.
The goal isn’t perfection. It’s moving from a state of constant crisis or quiet desperation to ordinary happiness. And for many people who’ve been struggling for years, ordinary happiness feels extraordinary. It’s about getting to a place where you’re not just reacting to emotional fires all day, but actually building something you care about.
Is DBT only for people with Borderline Personality Disorder?
Absolutely not. This is one of the biggest misconceptions about DBT.
Yes, Marsha Linehan originally developed DBT specifically for people with BPD. But here’s what we’ve learned over the past few decades: the skills work for anyone struggling with intense emotions or unhelpful behavioral patterns. The dialectical approach—balancing acceptance and change—is universally applicable.
We see remarkable results with DBT for PTSD, eating disorders, substance use, and chronic depression. It’s particularly effective for people who need more than once-a-week therapy but aren’t ready for inpatient treatment. If you find yourself feeling emotions more than others around you, or if you struggle with impulsive reactions when you’re upset, DBT might be exactly what you need—regardless of your diagnosis.
At Thrive Mental Health, we work with adults and young professionals across Florida with a wide range of challenges. Our virtual IOP programs are designed for anyone who needs structured, evidence-based support to build emotional regulation skills.
How can I get DBT treatment covered by my insurance?
Good news: many insurance plans cover DBT as part of Intensive Outpatient (IOP) or Partial Hospitalization (PHP) programs. We regularly work with Cigna, Optum, Florida Blue, and many other major carriers.
The first step is simple: verify your benefits to see what level of care your specific plan approves. Some plans require prior authorization, while others have specific criteria around diagnosis or medical necessity. It can feel overwhelming to steer insurance bureaucracy when you’re already struggling, which is why we handle most of this for you.
Our team at Thrive Mental Health can walk you through the verification process and help you understand your coverage. We operate across Florida, making evidence-based DBT treatment accessible whether you choose virtual or in-person care. The verification process usually takes just a few minutes, and there’s no obligation—we just want you to know what options are available.
Don’t let insurance confusion stop you from getting help. We’ve made it our mission to make this process as straightforward as possible.
Your Path to Balance Starts Here
You’ve made it this far, which means something brought you here—maybe confusion about therapy terms, maybe desperation for something that actually works, maybe both. Here’s what matters: understanding what does dialectical mean in dialectical behavior therapy isn’t just about memorizing a definition. It’s about finding a completely different way to move through your life.
The dialectical approach teaches us something revolutionary: you don’t have to choose. You don’t have to pick between accepting your pain and fighting for change. You don’t have to decide whether you’re “good enough as you are” or “need to be fixed.” Both can be true. Both are true.
This isn’t therapy-speak. It’s the practical foundation that helps people stop swinging between emotional extremes and start building lives that feel stable, meaningful, and genuinely worth living.
At Thrive Mental Health, we’ve watched this change happen hundreds of times. Our expert-led DBT programs bring these dialectical principles to life through structured, evidence-based treatment that meets you exactly where you are. Whether you’re struggling with intense emotions, self-harm, relationship chaos, or just feeling stuck in patterns that aren’t working—you can build a life with less crisis and more stability.
We operate across Florida, offering both virtual and in-person options because we know flexibility matters when you’re trying to get your life back on track. Our programs include evening sessions for young professionals and adults who can’t put their lives on hold for treatment.
Many of our clients use insurance coverage through Cigna, Optum, Florida Blue, and other major carriers to access our virtual IOP programs. We provide the level of care you need—more than once-a-week therapy, less than inpatient hospitalization—delivered by clinicians who actually understand what you’re going through.
You don’t have to figure this out alone. The dialectical truth? You’re doing the best you can right now, AND you deserve support to do even better.
Ready for support? Thrive offers virtual and hybrid IOP/PHP programs with evening options. Verify your insurance in 2 minutes (no obligation) or call 561-203-6085. If you’re in crisis, call/text 988.