CBT or DBT? How to Choose the Right Therapy for You

CBT vs DBT [2025]: Pick the Right Therapy in 5 Minutes (Save Time, Money, and Relapse)
CBT vs DBT—if you choose wrong, you can waste months and money. Choose right, and you can see relief in weeks. This 5-minute guide tells you exactly which one fits your symptoms, timeline, and budget.
What you’ll get:
- When to choose CBT vs DBT (in plain English)
- How long each takes and what each includes
- What results to expect—and how to start today using insurance
| Factor | CBT (Cognitive Behavioral Therapy) | DBT (Dialectical Behavior Therapy) |
|---|---|---|
| Best For | Anxiety, depression, OCD, phobias, PTSD | Borderline personality disorder, chronic suicidal thoughts, self-harm, intense emotional reactions |
| Primary Focus | Changing negative thought patterns | Accepting reality while regulating intense emotions |
| Session Structure | Weekly individual therapy (45-60 min) | Individual therapy + group skills training + phone coaching |
| Typical Duration | 6-20 weeks (short-term) | 6-12+ months (long-term) |
| Key Techniques | Cognitive restructuring, behavioral activation, exposure | Mindfulness, distress tolerance, emotion regulation, interpersonal effectiveness |
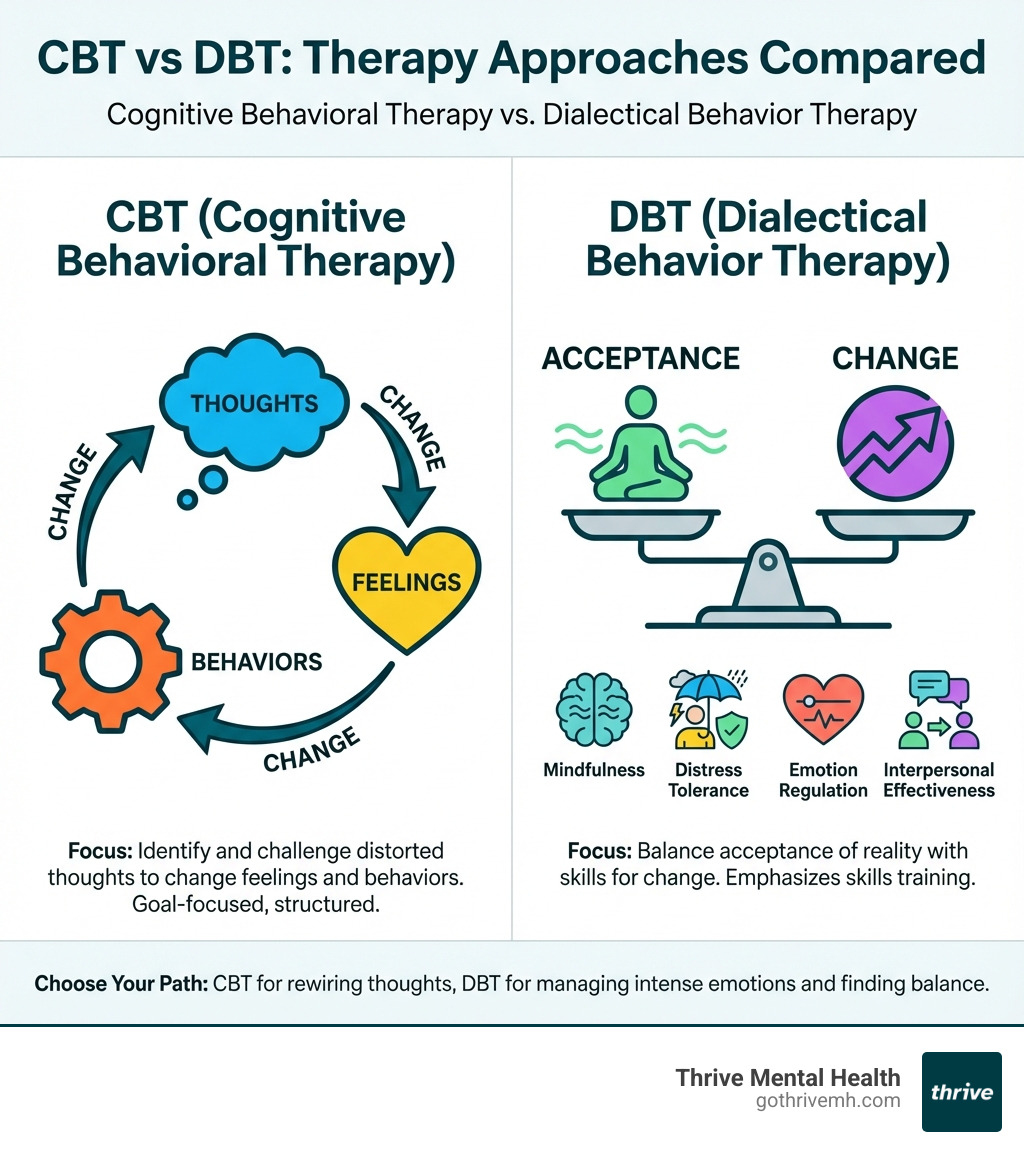
CBT helps you identify and challenge the distorted thoughts that fuel anxiety and depression. It’s direct, structured, and goal-focused—ideal if your main struggle is spiraling thoughts or avoidance behaviors.
DBT teaches you how to accept painful emotions without letting them control you. It’s designed for people who experience emotions so that they interfere with relationships, work, or safety. DBT combines acceptance with change, using skills like mindfulness and distress tolerance to help you ride out emotional storms.
Summary (CBT vs DBT): If your thoughts are the problem, CBT rewires them. If your emotions are overwhelming you, DBT gives you the tools to manage them. Use this guide to pick fast and start faster.
I’m Nate Raine, CEO of Thrive Mental Health. Our evidence-based programs, available to residents throughout Florida, integrate both CBT and DBT so you don’t waste time on the wrong fit.
This guide breaks down when each therapy works best, what to expect, and how to start with insurance support today.
Similar topics to cbt vs dbt:
- dialectical behavior therapy components
- how does dialectical behavioral therapy work
- what does dialectical behavior therapy treat
CBT vs. DBT: Two Paths to Rewire Your Brain
At Thrive Mental Health, we understand that effective mental wellness begins with understanding the root causes of distress. Both Cognitive Behavioral Therapy (CBT) and Dialectical Behavior Therapy (DBT) are powerful, evidence-based approaches, but they stem from different philosophical underpinnings and offer distinct tools for rewiring your brain and emotional responses.
Developed by Dr. Aaron T. Beck in the 1960s, CBT is rooted in the idea that our thoughts, feelings, and behaviors are interconnected. Its philosophical lineage draws from Stoicism and the Socratic Method, emphasizing logic and reason to challenge dysfunctional thought patterns. The goal is to help individuals identify and modify these patterns to improve their mental health.
DBT, on the other hand, emerged in the 1980s, developed by Dr. Marsha Linehan. While it builds upon CBT’s cognitive-behavioral framework, DBT integrates principles from Zen Buddhism and the concept of dialectics—the idea that two seemingly opposite things can be true at the same time. This means balancing acceptance of current reality with the need for change. DBT was initially created to address the intense emotional dysregulation seen in Borderline Personality Disorder (BPD), where traditional CBT alone proved insufficient.
How CBT Teaches You to Master Your Thoughts
CBT’s core principle is neatly simple yet profoundly effective: by changing how we think, we can change how we feel and act. Our thoughts aren’t just fleeting ideas; they deeply influence our emotions and subsequent behaviors. When we’re caught in a cycle of negative or distorted thinking, it can lead to significant distress.
The cognitive model in CBT helps us understand this interplay. It posits that an “activating event” (A) leads to our “beliefs” (B) about that event, which then results in “consequences” (C)—our emotional or behavioral response. The key insight here is that it’s often our interpretation (B), not the event itself (A), that determines our reaction (C).
In CBT, we work to identify these negative automatic thoughts and cognitive distortions. These are the unhelpful thinking patterns that can sabotage our well-being, such as:
- Catastrophizing: Blowing problems out of proportion (“If I fail this one task, I’ll lose my job and my life will be over!”).
- Overgeneralization: Drawing broad, negative conclusions from a single event (“I messed up that presentation, so I’m a complete failure at everything”).
- “Black-and-white” thinking: Seeing things in extremes, with no middle ground (“If I’m not perfect, I’m a total mess”).
Once identified, CBT provides concrete techniques to challenge these thoughts. We learn to evaluate their accuracy and usefulness, asking questions like: “What’s the evidence for this thought?” or “Is there another way to look at this situation?” This process of cognitive restructuring helps replace unhelpful thoughts with more balanced, realistic ones.
Beyond thought work, CBT also incorporates behavioral strategies. Behavioral activation encourages engaging in positive activities, even when motivation is low, to improve mood. Problem-solving skills equip us to tackle life’s stressors effectively, reducing feelings of helplessness. Through these structured, goal-oriented techniques, CBT empowers individuals to become their own therapists, mastering their thoughts and changing their mental health. To learn more about this transformative process, explore How CBT Can Transform Negative Thought Patterns.
How DBT Teaches You to Master Your Emotions
While CBT excels at addressing thought patterns, DBT steps in when emotions become overwhelmingly intense, making it difficult to function or even stay safe. DBT, a specialized form of CBT, is built on the premise that some individuals experience emotions with extreme intensity and volatility, often leading to impulsive or destructive behaviors.
The core of DBT is a delicate balance between acceptance and change. We recognize that individuals need to accept their current reality and emotions, no matter how painful, while simultaneously working towards changing problematic behaviors and developing healthier coping mechanisms. This “dialectical” approach acknowledges that opposing truths can coexist.
A cornerstone of DBT is validation. This isn’t about agreeing with destructive behaviors, but rather acknowledging that a person’s feelings, thoughts, and actions make sense within their life context. For someone who has experienced trauma, for instance, intense emotional reactions might be a logical, albeit unhelpful, response to their past. Validation helps reduce shame and fosters a safe environment for change.
Linehan’s biosocial theory helps explain the origins of emotional dysregulation. It suggests that some individuals are biologically predisposed to emotional sensitivity, and when combined with an “invalidating environment” (where their emotional experiences are consistently dismissed or punished), they struggle to learn healthy emotion regulation skills.
DBT addresses this by teaching individuals concrete skills to manage intense emotions, improve relationships, and tolerate distress. It’s a comprehensive program designed to help individuals with emotional dysregulation move from a state of chronic crisis to building a life worth living. To dig deeper into how this powerful therapy works, explore How Does Dialectical Behavior Therapy Work?.
The Core Differences: A Head-to-Head Comparison of CBT vs DBT
While both CBT and DBT are potent forces in mental health, they are custom for different purposes. Think of it like this: if you’re battling a persistent cough, you might need a general cold medicine. But if you have severe asthma, you need a specialized inhaler. Both address respiratory issues, but one is designed for a more intense, chronic condition. This table highlights their distinct features:
| Feature | Cognitive Behavioral Therapy (CBT) | Dialectical Behavior Therapy (DBT) |
|---|---|---|
| Primary Focus | Identifying and changing unhelpful thought patterns that lead to distress and problematic behaviors. | Balancing acceptance of current reality and intense emotions with skills for change; managing emotional dysregulation. |
| Key Techniques | Cognitive restructuring, behavioral activation, exposure therapy, psychoeducation, problem-solving. | Mindfulness, Distress Tolerance, Emotion Regulation, Interpersonal Effectiveness. |
| Treatment Structure | Typically individual weekly sessions (45-60 minutes). Can be delivered in groups or virtually. | Comprehensive program including individual therapy (weekly, 50 min), weekly group skills training (2-2.5 hours), phone coaching for crisis, and therapist consultation team meetings. |
| Typical Duration | Short-term, usually 6-20 weeks (e.g., 12-16 weeks for many conditions). | Longer-term, typically 6-12+ months to complete all modules, often 1-1.5 years. |
| Therapeutic Relationship | Collaborative, often structured and directive, with the therapist guiding the client in identifying and challenging thoughts. | Validating, coaching-oriented, emphasizes radical acceptance, with the therapist providing direct support and guidance in skill application, especially during crises. |
| Philosophical Roots | Stoicism, Socratic Method (logic, reason). | Zen Buddhism (mindfulness, acceptance), Dialectics (synthesis of opposites). |
| Homework | Essential for practicing skills and tracking thoughts/behaviors between sessions. | Essential for practicing skills learned in group and individual sessions, often using diary cards. |
The 4 Unbreakable Skills DBT Teaches You
DBT stands out for its structured, skill-based approach, delivered through four core modules. These aren’t just concepts; they are practical, actionable strategies designed to fundamentally change how you experience and respond to intense emotions.
- Mindfulness: This skill teaches you to be fully present and aware in the moment, without judgment. It’s about observing your thoughts, feelings, and sensations as they happen, helping you detach from overwhelming emotions and gain perspective. Mindfulness practices, often drawn from Zen traditions, are integrated throughout DBT to cultivate a sense of calm and presence.
- Distress Tolerance: When you’re in the midst of an emotional crisis, the urge to react impulsively or destructively can be immense. Distress Tolerance skills equip you to cope with intense, uncomfortable emotions and situations without making things worse. Techniques like self-soothing, intense exercise, controlled breathing, and progressive muscle relaxation help you ride out emotional waves until they subside.
- Emotion Regulation: This module focuses on understanding, managing, and expressing your emotions in healthy ways. We learn to identify emotions, understand their function, reduce emotional vulnerability, and change unwanted emotions. The goal isn’t to eliminate emotions, but to reduce their intensity and duration, preventing them from controlling your life.
- Interpersonal Effectiveness: Relationships are often a source of both joy and pain. This module teaches you how to steer social situations more skillfully, assert your needs, set healthy boundaries, and maintain self-respect. It helps you communicate effectively and build stronger, more stable relationships.
These four modules are taught in a group setting, allowing clients to practice new behaviors and receive feedback in a supportive environment, and then reinforced in individual therapy. For a comprehensive look at how these skills are developed, explore Dialectical Behavior Therapy Components.
The ABCs of Changing Your Mind with CBT
CBT provides a clear, actionable framework for understanding and altering the connection between our thoughts, feelings, and behaviors. A foundational model in CBT, particularly from Albert Ellis’s Rational Emotive Behavior Therapy (REBT), is the ABC Model.
- A – Activating Event: This is the objective situation or event that occurs. It could be anything from receiving an email to a social interaction or even an internal thought.
- B – Beliefs: This is our interpretation or evaluation of the activating event. Our beliefs are often automatic and can be rational or irrational, helpful or unhelpful. They are the lens through which we view the world.
- C – Consequences: These are the emotional and behavioral reactions that follow from our beliefs about the event.
The power of the ABC Model lies in its ability to highlight that our emotional and behavioral consequences (C) are not directly caused by the activating event (A), but rather by our beliefs (B) about that event. For example, if you receive a critical email (A), your belief that “I’m a failure” (B) might lead to feelings of intense sadness and withdrawal (C). However, if your belief was “This is feedback I can learn from” (B), your consequence (C) might be motivation to improve.
CBT leverages this understanding through cognitive restructuring techniques. We work collaboratively to:
- Identify your automatic thoughts and beliefs in response to various situations.
- Challenge these beliefs by examining the evidence for and against them, considering alternative explanations, and evaluating their usefulness.
- Replace unhelpful or distorted beliefs with more balanced, realistic, and adaptive thoughts.
This process empowers you to gain control over your emotional reactions and behaviors by first gaining control over your thoughts. To dive deeper into the practical applications of CBT, check out A Beginners Guide to Cognitive Behavioral Therapy (CBT).
Which Therapy Wins for Anxiety, BPD, or Depression?
If you are in crisis or having thoughts of self-harm, call or text the 988 Suicide & Crisis Lifeline. You are not alone.
Callout: If you’re in crisis, call/text 988 right now. You are not alone.
Choosing between CBT and DBT often comes down to the specific mental health conditions you’re facing. While there’s overlap, each therapy has its “sweet spot” where it demonstrates exceptional efficacy. Understanding these distinctions is crucial for selecting a treatment that delivers real, measurable results.

When CBT Is the Gold Standard
CBT is widely recognized as a “gold standard” in psychotherapy due to the vast amount of evidence-based research supporting its effectiveness. It’s often the first-line treatment recommended for a broad range of conditions, especially those where negative thought patterns play a significant role.
- Anxiety Disorders: CBT is strongly effective for anxiety disorders, including Panic Disorder, Generalized Anxiety Disorder, Social Phobia, and Obsessive-Compulsive Disorder (OCD). Research on cognitive-behavioral treatments for anxiety and stress-related disorders has confirmed its effectiveness, even when delivered online, showing large effect size reductions in anxiety and depression symptom severity.
- Depression: For mild to moderate depressive episodes, CBT has a large evidence base demonstrating its efficacy. It’s particularly effective when paired with medication for more severe cases. CBT helps individuals challenge thoughts of worthlessness or hopelessness, replacing them with more balanced perspectives.
- PTSD: CBT, particularly trauma-focused variations like Cognitive Processing Therapy (CPT), is highly effective in improving symptoms for people with Post-Traumatic Stress Disorder.
- Other Conditions: CBT also shows promise for anger problems, drug abuse, general stress, insomnia, bulimia, fibromyalgia, chronic fatigue syndrome, smoking cessation, gambling, and irritable bowel syndrome (IBS).
If you’re struggling with persistent worries, panic attacks, phobias, or the heavy weight of depression, CBT offers a structured, goal-oriented path to relief. To dig deeper into how CBT combats anxiety and depression, read our guide: Cognitive Behavioral Therapy: A Deep Dive into How it Battles Anxiety and Depression.
When DBT Is the Front-Line Defense
DBT was born out of a necessity to treat conditions that traditional CBT struggled with, particularly those characterized by extreme emotional dysregulation and high-risk behaviors. It has since become the front-line defense for several complex mental health challenges.
- Borderline Personality Disorder (BPD): DBT is the only empirically supported treatment for BPD and is often recommended as a first-line treatment. A meta-analysis of DBT’s effectiveness on BPD found significant reductions in suicidal ideation, self-injurious behavior, depression, and anxiety. One study even found that after a year of DBT, around 77% of patients no longer met the criteria for a BPD diagnosis. It’s been shown to reduce the need for medical care and medication by as much as 90% for BPD.
- Chronic Suicidal Ideation and Self-Harm Behaviors: DBT was specifically developed for suicidal individuals and those engaging in self-harm. Its emphasis on distress tolerance and emotion regulation skills provides crucial tools for managing intense urges without resorting to destructive actions.
- Complex PTSD: For individuals with complex trauma who experience severe emotional dysregulation, DBT-PTSD (a specialized form of DBT) has shown to be highly effective, even compared to other trauma-focused therapies like CPT. It helps individuals manage overwhelming emotions that often accompany trauma.
- Eating Disorders & Substance Use Disorders: DBT is also effective for these conditions, as they often involve intense emotional experiences and impulsive behaviors. It helps individuals develop healthier coping mechanisms and reduce maladaptive patterns.
- ADHD: While initially developed for BPD, DBT has evolved and is now recognized as a valuable tool for managing adult ADHD, particularly due to its focus on mindfulness, emotion regulation, and distress tolerance, which can help with impulsivity and emotional control.
- Other Conditions: DBT has also shown promise in reducing depressive symptoms and anxiety in various populations, and for improving affective control in those with bipolar disorder.
If you’re living with intense emotions that feel uncontrollable, struggling with self-harm, chronic suicidal thoughts, or navigating complex relationship dynamics due to emotional volatility, DBT offers a comprehensive and life-changing pathway to stability and a life worth living. To explore how DBT can improve mental health for these challenging conditions, visit How Dialectical Behavior Therapy (DBT) Can Improve Mental Health.
Making Your Choice: Is CBT or DBT Right for Your Recovery?
Deciding between CBT vs DBT can feel like standing at a crossroads. Both therapies offer powerful tools for healing and growth, but the “right” choice is deeply personal. It depends on your unique needs, your readiness for change, and the specific challenges you’re looking to overcome. At Thrive Mental Health, we are dedicated to helping Floridians make an informed decision for their recovery journey.
Questions to Ask Before You Commit
Before you commit to a specific therapy, taking a moment for self-reflection can illuminate the path forward. Ask yourself these critical questions:
- What are my primary symptoms or challenges? Am I primarily struggling with persistent negative thoughts, anxiety, or specific phobias? Or are my emotions so intense and overwhelming that they lead to impulsive behaviors, self-harm, or unstable relationships?
- How do I typically handle intense emotions? Do I tend to suppress them, get caught in thought spirals, or do they feel so powerful that I react in ways I later regret?
- What kind of time commitment am I ready for? Am I looking for a more short-term, focused intervention (typically 6-20 weeks), or am I prepared for a longer, more comprehensive program that might last 6-12 months or more?
- Do I prefer individual or group settings? While both therapies include individual sessions, DBT’s comprehensive model heavily relies on group skills training. How do I feel about learning and practicing skills in a group?
- What are my goals for therapy? Am I seeking to change specific thought patterns and behaviors, or do I need to learn to accept difficult emotions while building a life worth living?
Your answers to these questions can provide valuable insights into which therapy might align better with your current needs and preferences. For a deeper understanding of how these therapies integrate into more intensive programs, explore Navigating Intensive Outpatient Therapy: The Roles of CBT and DBT Explained.
How a Professional Can Pinpoint Your Needs
While self-assessment is helpful, the most effective way to determine if CBT or DBT is the best fit for you is through a comprehensive diagnostic assessment with a qualified mental health professional. Our team of experts at Thrive Mental Health specializes in tailoring personalized treatment plans for Florida residents based on your unique history, symptoms, and goals.
A skilled therapist will:
- Conduct a thorough evaluation: This includes understanding your current symptoms, mental health history, and any co-occurring conditions. For instance, someone with ADHD might benefit from DBT’s emotion regulation skills alongside CBT’s organizational strategies.
- Discuss your readiness for change: Some individuals are ready for direct change-oriented work, while others first need to develop skills for emotional stability before tackling deeper issues.
- Consider an integrated approach: Often, the most powerful treatment combines elements of both CBT and DBT. For instance, a client might start with DBT to stabilize intense emotions and reduce self-harm, then transition to CBT to address specific cognitive distortions or trauma. This blended approach is common in our Florida-based Intensive Outpatient (IOP) and Partial Hospitalization (PHP) programs.
- Review treatment structure and duration: We’ll help you understand the commitment involved with each therapy and how it fits into your life. Thrive Mental Health offers flexible virtual and in-person programs across Florida, designed for people who need more than once-a-week therapy but less than inpatient care.
- Clarify insurance coverage: We work with major providers like Cigna, Optum, and Florida Blue, among others, to make evidence-based treatment accessible. Verify your insurance in 2 minutes, no obligation.
Whether you’re seeking to overcome anxiety and depression with CBT, or manage intense emotions and build a life worth living with DBT, our Florida-focused programs are designed to deliver measurable results. We offer specialized virtual IOPs for both CBT Virtual IOP and DBT Virtual IOP, ensuring you receive expert-led care customized to your needs, no matter where you are in the Sunshine State.
Frequently Asked Questions about CBT vs DBT
What’s the biggest difference between CBT and DBT?
CBT changes unhelpful thoughts; DBT balances acceptance with change to manage intense emotions and impulsive behaviors.
Which works faster—CBT or DBT?
Usually CBT. Many people see results in 12–20 weeks. DBT is longer (6–12+ months) because it teaches a full skill set for emotion regulation and safety.
Is DBT only for Borderline Personality Disorder?
No. DBT also helps with chronic suicidality, self-harm, complex PTSD, eating disorders, substance use, and ADHD-related emotional dysregulation.
Can I combine CBT and DBT?
Yes. Many start with DBT for stability and safety, then use CBT to target specific thoughts and behaviors.
Will insurance cover CBT or DBT?
Often yes. Thrive works with major Florida providers like Cigna, Optum, and Florida Blue. Check your benefits in 2 minutes.
Ready for support? Thrive offers virtual and hybrid IOP/PHP programs across Florida, with evening options available. Verify your insurance in 2 minutes (no obligation) → Start benefits check or call our Florida-based team at 561-203-6085. If you’re in crisis, call/text 988.