Depression Symptoms: What to Watch For in Yourself and Others

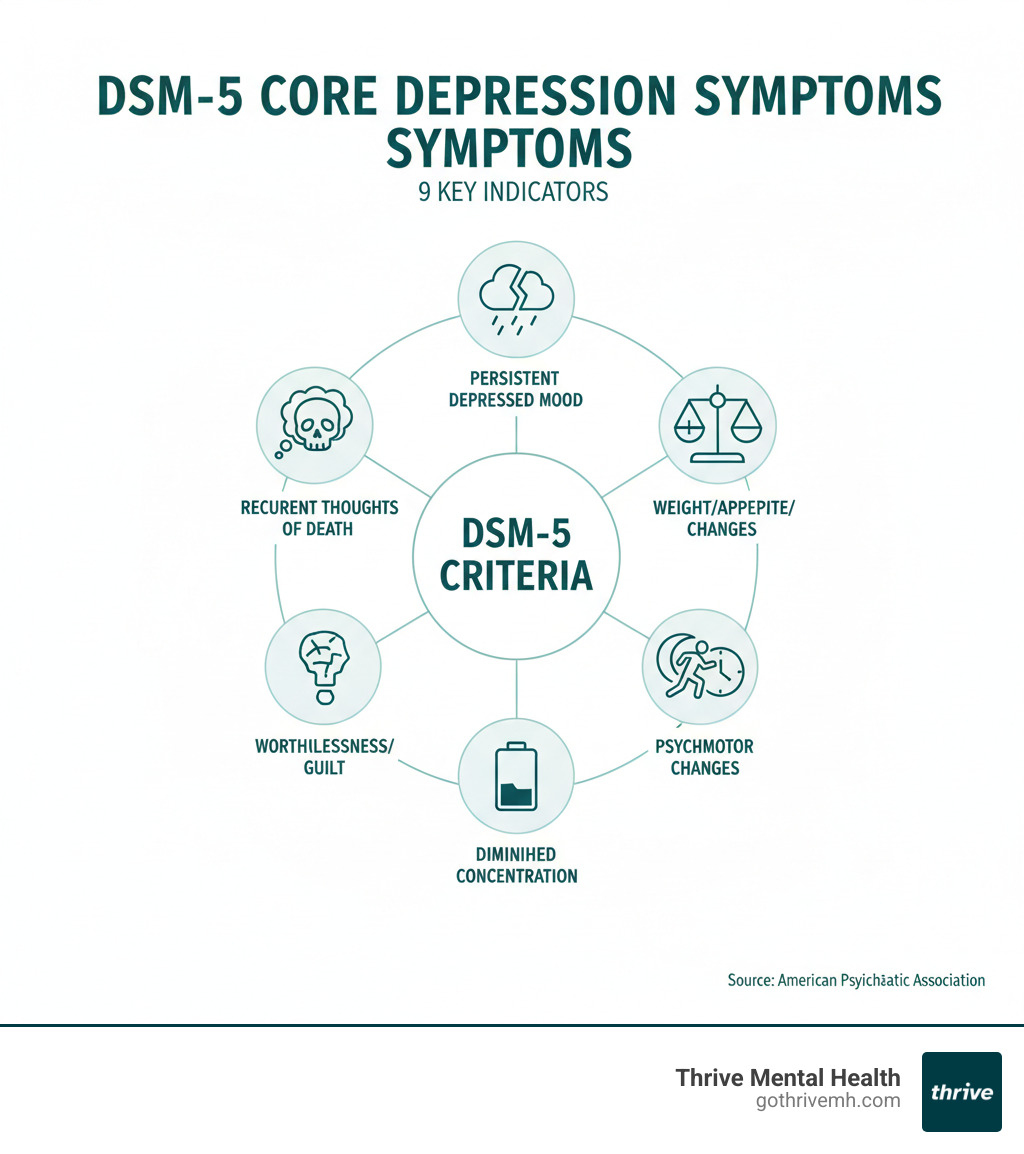
Depression Symptoms: Uncover 9 Core Warning Signs
CRISIS SUPPORT: If you’re in immediate danger or having thoughts of self-harm, call or text 988 or chat at 988lifeline.org. You are not alone.
If you’re in crisis, call/text 988 right now. You are not alone.
Depression Symptoms: 9 Signs You Can’t Ignore—and How to Feel Better Faster
Summary: Depression symptoms are more than sadness—recognize the 9 core signs early to get effective treatment faster and feel better sooner.
Depression symptoms go far beyond feeling sad. While sadness is a normal human emotion, clinical depression is a persistent and serious medical condition that affects how you feel, think, and handle daily activities.
The most common depression symptoms include:
- Persistent sadness or empty mood
- Loss of interest or pleasure in activities
- Significant changes in appetite or weight
- Sleep disturbances (insomnia or sleeping too much)
- Fatigue or loss of energy
- Feelings of worthlessness or excessive guilt
- Difficulty concentrating or making decisions
- Slowed movements or restless behavior
- Recurrent thoughts of death or suicide
Depression affects more than 16% of U.S. adults at some point in their lifetime and can affect anyone regardless of age, race, or income. Recognizing these symptoms is the first crucial step toward getting help. Depression is highly treatable, and with proper support, recovery is not only possible but likely.
The Core Emotional and Behavioral Depression Symptoms
Depression symptoms create a complex web of emotional and behavioral changes. Understanding these psychological signs is crucial because they often appear before someone realizes they’re dealing with depression.
Key Psychological Symptoms of Depression
The emotional landscape of depression feels like living under a heavy, gray blanket that muffles everything that once brought joy.
Persistent sadness or empty mood is a deep, continuous feeling that lasts most of the day, nearly every day, for at least two weeks. Some describe it less as sadness and more as feeling completely empty.
Loss of interest or pleasure (anhedonia) is when activities you once loved, from hobbies to socializing, feel pointless or like a chore.
Feelings of worthlessness or excessive guilt involve taking blame for things that aren’t your fault, feeling like a burden, or believing you’re fundamentally flawed.
Hopelessness and pessimism create a tunnel vision where the future looks bleak and it feels impossible for things to improve.
Difficulty concentrating or making decisions, often called “brain fog,” makes simple tasks like reading or making choices feel impossible.
For a deeper understanding of how depression differs from other mood conditions, check out our guide on Decoding Bipolar and Depression: Comprehensive Definitions.
Behavioral Changes to Watch For

While the internal experience of depression is invisible, it often shows up in observable ways. These behavioral depression symptoms can be early warning signs.
Irritability, frustration, or angry outbursts are often overlooked. Depression can manifest as snapping at loved ones or having zero tolerance for minor annoyances, especially in men.
Social withdrawal and isolation often happens gradually, starting with skipping social events and leading to avoiding friends and family entirely.
Neglecting responsibilities or personal hygiene occurs when depression saps energy, making basic tasks like showering, laundry, or work feel monumental. This is a symptom, not laziness.
Increased use of alcohol or drugs can develop as a way to cope with emotional pain, escalating into a pattern of self-medication.
High-risk or escapist behaviors are attempts to feel something other than emptiness and can include reckless driving, impulsive spending, or other uncharacteristic dangerous activities.
Recognizing these behavioral changes is often the first step toward getting help. These symptoms aren’t character flaws; they’re signs that professional support could make a real difference.
The Unseen Physical Toll of Depression
Depression symptoms aren’t just “in your head.” Depression creates a cascade of physical changes, and these are often the first signs people notice.
Common Physical Symptoms
Your body has its own way of expressing emotional distress, and depression symptoms often show up in surprisingly physical ways.

Chronic fatigue and low energy is a profound exhaustion that doesn’t improve with sleep. People often describe it as feeling “bone-tired,” making simple tasks overwhelming.
Sleep disturbances are common, manifesting as either insomnia (difficulty sleeping) or hypersomnia (sleeping too much). In either case, you still wake up feeling unrested.
Significant appetite or weight changes can go in either direction. Some people lose their appetite and lose weight, while others turn to food for comfort and gain weight. A change of more than 5% in a month is clinically significant.
Unexplained aches, pains, headaches, or cramps are surprisingly common. Depression can cause chronic backaches or persistent headaches that don’t respond to typical pain relievers.
Digestive issues like constipation, diarrhea, or nausea can be triggered by depression due to the gut-brain axis. Since most of the body’s serotonin is in the gut, mood and digestive problems are often linked. Scientific research on the gut-brain connection continues to reveal this link.
Less-Recognized Physical Signs
Some physical depression symptoms fly under the radar because they are not commonly discussed.
Decreased sex drive is a common but often underreported symptom that can strain relationships and add to emotional distress.
Slower movements or speech, known as psychomotor retardation, involves noticeably slower physical actions and speech that can make social interactions difficult.
Weakened immune system can result from the chronic stress and inflammation caused by depression. You might notice you’re catching more colds or taking longer to recover from illness.
How Depression Symptoms Change Across a Lifetime
Depression symptoms are not one-size-fits-all; they shift depending on a person’s age and life stage. Understanding these variations is key to getting help early.
In Children and Teens
Spotting depression symptoms in young people is challenging, as they often hide behind what looks like typical growing pains. Approximately 4.4% of U.S. children have been diagnosed with depression.
- Irritability and anger are often more common than sadness. Kids and teens may lash out or seem constantly agitated.
- Physical complaints like stomach aches or headaches, especially on school days, can be a sign in younger children.
- Poor school performance, such as a sudden drop in grades or skipping classes, is a major red flag.
- Social withdrawal from friends, family, and activities they once enjoyed is common.
- Sensitivity to rejection can become heightened, making peer relationships difficult.
Black teenagers face unique challenges and are more likely to attempt suicide than white teenagers, highlighting how systemic issues can intensify these struggles. For more information, see the NIMH information on teen depression.
In Older Adults
Depression symptoms in older adults are often mistakenly dismissed as a normal part of aging. Depression is a medical condition, not an inevitable part of getting older.
- Unexplained physical pain is a common complaint. Instead of saying they feel sad, older adults may report chronic aches or digestive issues.
- Memory difficulties and personality changes can be mistaken for dementia. They might struggle to remember appointments or seem confused.
- Apathy and lack of motivation can lead them to lose interest in hobbies, family gatherings, and other activities they once enjoyed.
- Social isolation often creeps in as they decline invitations and withdraw from community activities.
Recognizing that these are not inevitable parts of aging is crucial. The NIMH information on depression in older adults provides valuable guidance.
Types of Depression and When to Seek Help
Understanding the specific type of depressive disorder you’re experiencing guides you toward the most effective treatment. It’s also critical to know when depression symptoms require professional intervention.
Different Depressive Disorders
The DSM-5 recognizes several distinct forms of depression, each with unique patterns.
- Major Depressive Disorder (MDD): Characterized by at least five severe depression symptoms (including sadness or loss of pleasure) for at least two weeks, significantly disrupting daily life.
- Persistent Depressive Disorder (Dysthymia): A less intense but chronic form of depression where symptoms persist for at least two years.
- Seasonal Affective Disorder (SAD): Follows a seasonal pattern, typically emerging during the shorter, darker days of fall and winter.
- Peripartum (Postpartum) Depression: Affects new mothers during pregnancy or in the weeks after childbirth, going far beyond the “baby blues.”
- Premenstrual Dysphoric Disorder (PMDD): A severe form of PMS with intense mood changes and depression symptoms the week before menstruation.
When to Get Professional Help
Knowing when to reach out for professional support is crucial. Depression rarely resolves on its own.
Crisis Support: If you or someone you know is in crisis or having thoughts of suicide, call or text the 988 Suicide & Crisis Lifeline at 988 or chat at 988lifeline.org. You are not alone.
You should seek help when:
- Symptoms last more than two weeks and dominate most of your day.
- Symptoms interfere with work, school, or relationships, impairing your ability to function.
- You have any thoughts of self-harm or suicide. This is an emergency and requires immediate attention.
- Lifestyle changes aren’t helping. Self-care is supportive but often not enough for clinical depression.
At Thrive Mental Health, our Areas of Care: Virtual IOP – Depression programs provide structured support when you need more than weekly therapy.
Treatment Options and Insurance
The encouraging truth is that depression is highly treatable. With the right approach, recovery is probable.
- Psychotherapy (talk therapy) helps you work with a professional to change unhelpful thought patterns. Methods like Cognitive Behavioral Therapy (CBT) are highly effective.
- Medication, such as antidepressants, can help rebalance brain chemistry and is often most effective when combined with therapy.
- Intensive Outpatient (IOP) and Partial Hospitalization (PHP) offer structured treatment while you live at home, ideal for when symptoms are severe.
- Virtual therapy lets you get expert care from home. Learn more: Virtual Therapy.
- Lifestyle changes like exercise, nutrition, and social connection are powerful allies in recovery.
Not sure what your plan covers? Verify your insurance in 2 minutes—no obligation.
Approximately 80% to 90% of people who seek treatment respond well. We know navigating care can be overwhelming. Many insurance plans, including Cigna, Optum, and Florida Blue, provide coverage for mental health treatment. Thrive Mental Health is proud to serve residents throughout Florida, making expert-led care accessible across the state.
Frequently Asked Questions about Depression Symptoms
When people start recognizing depression symptoms, they naturally have questions. Here are clear, compassionate answers to the most common ones.
What are the 5 main symptoms of depression?
While a clinical diagnosis requires at least five symptoms from a broader list, five of the most common and impactful depression symptoms are:
- Persistent depressed mood: A deep, empty feeling that lasts most of the day, nearly every day.
- Loss of interest or pleasure (anhedonia): Losing interest in hobbies, social activities, or work.
- Significant appetite or weight changes: Either eating much more or much less, leading to weight gain or loss.
- Sleep disturbances: Insomnia (can’t sleep) or hypersomnia (sleeping too much) while still feeling tired.
- Chronic fatigue: A profound loss of energy that isn’t relieved by rest.
How do I know if I’m depressed or just sad?
The key differences are duration, pervasiveness, and impairment. Sadness is a temporary and specific reaction to an event. You can still experience moments of joy. Depression is a persistent illness lasting at least two weeks, where feelings of emptiness and hopelessness are constant and interfere with your ability to function at work, school, or in relationships. Even when good things happen, the low mood remains.
Can depression go away on its own?
While a mild, brief low mood might improve, clinical depression is a serious medical condition that rarely goes away without treatment. Untreated depression often worsens over time and can increase the risk of other health problems and suicidal thoughts. Seeking professional help is a courageous and necessary step for recovery. The good news is that depression is highly treatable, with 80-90% of people responding well to proper care.
What is the first sign of depression most people notice?
Often it’s a loss of interest in things that used to feel rewarding, or unusual fatigue that doesn’t lift with sleep. These early depression symptoms can appear before persistent sadness.
When should I see a doctor vs. go to the ER for depression symptoms?
- Go to the ER or call/text 988 immediately if you have thoughts of self-harm, suicide, or feel unsafe. You are not alone.
- See a doctor or therapist if symptoms last 2+ weeks, or they disrupt work, school, sleep, appetite, or relationships.
Take the First Step Toward Feeling Better
Ready for support in Florida? Thrive offers virtual and hybrid IOP/PHP with evening options. Verify your insurance in 2 minutes (no obligation) or call 561-203-6085. If you’re in crisis, call/text 988.