Beyond the Trauma: Is PTSD Truly a Mental Illness?

Is PTSD a mental illness? 4 Crucial Facts
Why Understanding PTSD as a Mental Illness Matters
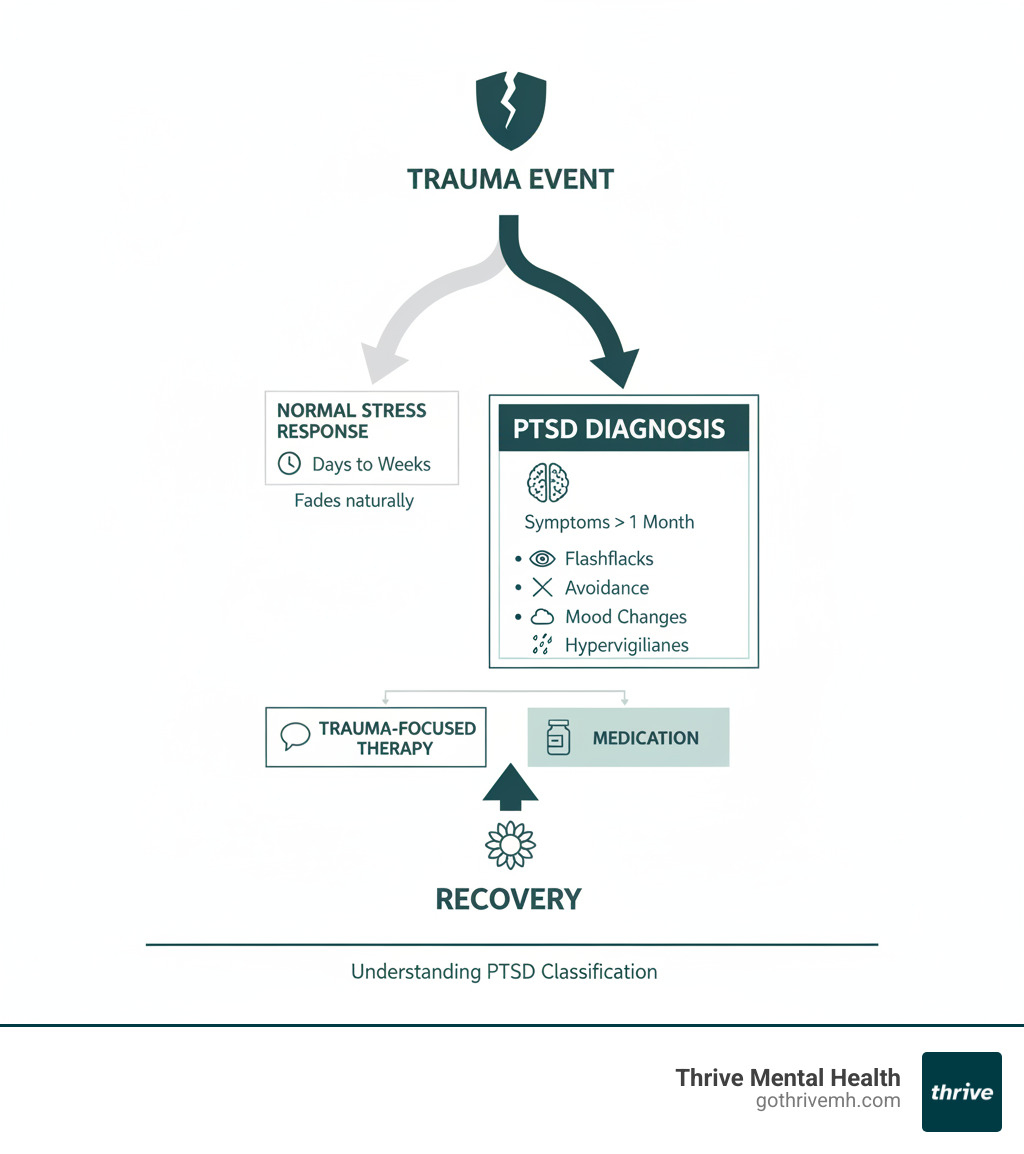
Is PTSD a mental illness? Yes, Post-Traumatic Stress Disorder (PTSD) is a recognized mental health condition, classified in the DSM-5 as a trauma- and stressor-related disorder.
Quick Answer:
- PTSD is a mental illness – officially diagnosed when symptoms last over a month.
- It’s treatable – trauma-focused therapy and medication are effective.
- It’s not your fault – PTSD involves biological changes in the brain after trauma.
- Insurance covers it – most plans pay for evidence-based PTSD treatment.
It’s normal to feel stressed or anxious after a traumatic event. However, when these reactions don’t fade after a month and interfere with work, relationships, or daily life, it may be PTSD.
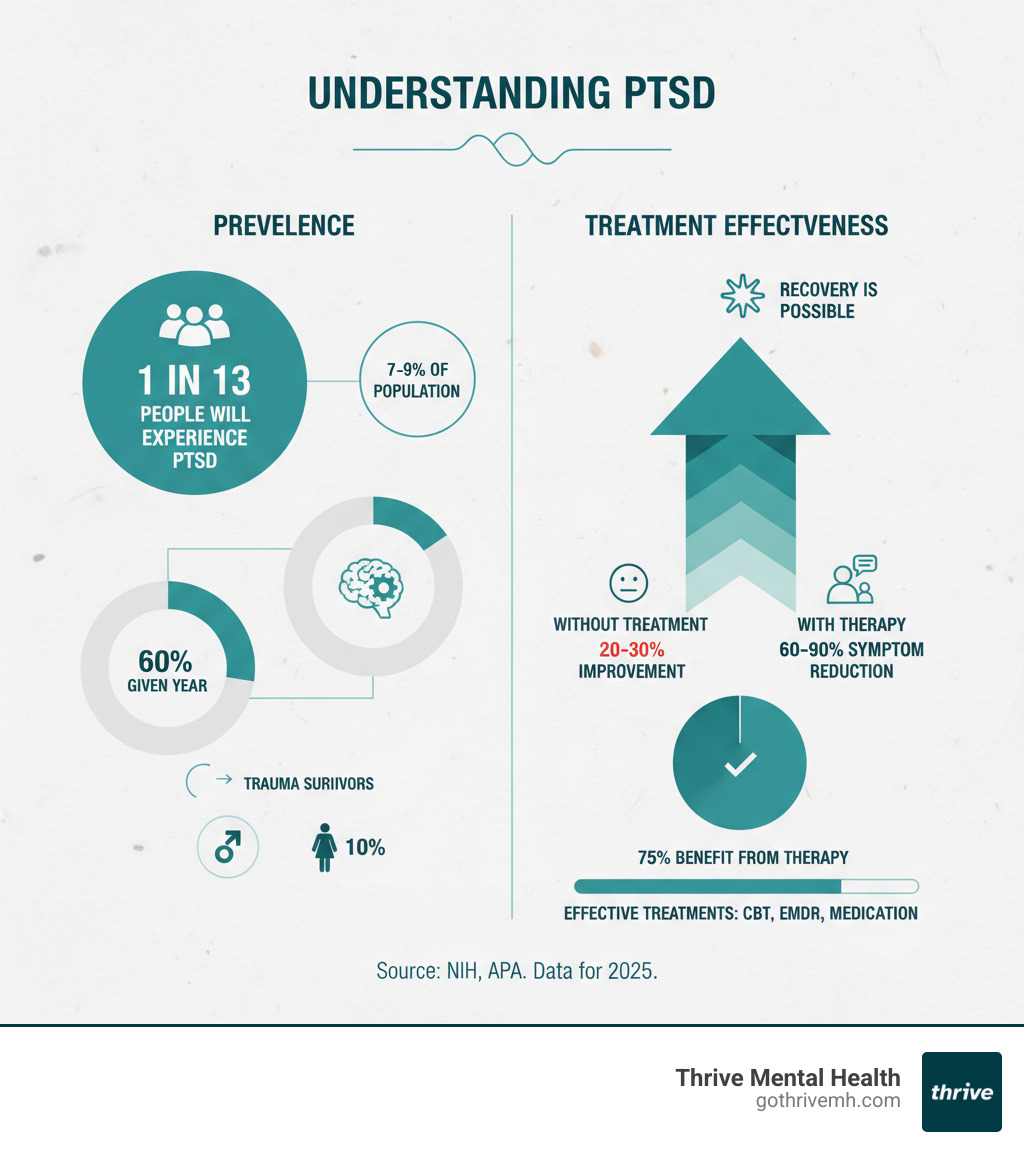
The difference isn’t about being “strong” or “weak.” PTSD is a medical condition that affects about 6% of adults in their lifetime. It develops when trauma overwhelms the brain’s ability to process what happened, leading to persistent symptoms.
Understanding that PTSD is a legitimate mental illness is crucial. It reduces stigma, validates your suffering, and opens access to proven treatments. You’re not “just stressed”—you have a treatable condition that responds well to professional care.
Basic is ptsd a mental illness glossary:
What Are the Real Symptoms of PTSD? [4 Key Clusters Explained]
![Visual of PTSD symptom clusters. Alt text: “PTSD symptoms: intrusion, avoidance, mood, arousal”]
Is PTSD a mental illness with clear symptoms? Absolutely. It’s a specific mental health condition with four distinct symptom clusters used for diagnosis. To qualify, symptoms must last more than a month and seriously interfere with daily life, making it hard to work or maintain relationships.
How long do symptoms last? Without treatment, PTSD can persist for years, but with proper care, symptoms can improve significantly.
How PTSD disrupts daily life can include replaying a traumatic scene during a work meeting, avoiding entire neighborhoods, or constantly checking locks before bed.
Here’s how PTSD shows up, broken down into the four main symptom groups:
1. Intrusion & Re-Experiencing
This cluster involves the trauma feeling like it’s happening again. Flashbacks feel real, pulling you back to the event. Nightmares about the trauma can lead to insomnia. Unwanted memories can surface at any time, and emotional and physical reactions to triggers (like a loud noise) can be overwhelming, causing a racing heart or shortness of breath.
2. Avoidance
This involves trying to escape reminders of the trauma. You might avoid people, places, or activities connected to the event. This can also manifest as emotional numbness, where you feel detached from your own life and unable to experience positive emotions like joy or love, leading to isolation.
3. Negative Mood & Thinking
Trauma can distort your view of yourself and the world. This includes persistent guilt and shame, blaming yourself for what happened. You may have memory gaps related to the trauma. A feeling of detachment from friends and family is common, as is a loss of interest in hobbies and activities you once enjoyed.
How PTSD Impacts Daily Life: The Role of Flashbacks, Avoidance, and Anxiety
4. Arousal & Reactivity Changes
Your nervous system remains on high alert. Hypervigilance means constantly scanning for danger and being easily startled. You might experience uncharacteristic irritability and anger. Sleep and focus problems are common, leaving you exhausted yet unable to rest or concentrate. Some people engage in self-destructive behaviors like substance abuse or reckless driving to cope. These are not character flaws but symptoms of a brain trying to protect itself. Treatment can significantly improve these reactions.
Related: Understanding the Symptoms Associated with PTSD
Is PTSD a Mental Illness? [What the Experts Say]
Yes, PTSD is officially recognized as a mental illness. Since 1980, the American Psychiatric Association has classified it in the Diagnostic and Statistical Manual of Mental Disorders (DSM). In the current DSM-5, PTSD was moved to its own category: trauma- and stressor-related disorders. This change acknowledged its unique origins and symptoms, distinguishing it from anxiety disorders.
The medical consensus is clear: PTSD is a disease, not just a “reasonable reaction” to trauma, due to its persistent, life-disrupting nature and its effects on brain function.
How Do Professionals Diagnose PTSD?
A professional diagnosis is essential and involves a thorough clinical assessment based on DSM-5 criteria. A diagnosis requires exposure to a traumatic event (actual or threatened death, serious injury, or sexual violence).
A professional then looks for a specific combination of symptoms from the four clusters:
- At least one intrusion symptom (e.g., flashbacks, nightmares)
- At least one avoidance symptom
- At least two negative mood changes (e.g., guilt, detachment)
- At least two arousal changes (e.g., hypervigilance, sleep problems)
These symptoms must last more than one month and cause significant distress or impairment in daily life. A proper diagnosis validates your experience and is the first step toward effective treatment.
Understanding Post-Traumatic Stress Disorder (PTSD) Symptoms, Causes, and Treatment Options
Why the Label “Mental Illness” Matters
Calling PTSD a “mental illness” is important. It reduces stigma by framing it as a medical condition, not a personal failing. It validates suffering, confirming that your symptoms are real reactions to trauma. Crucially, the official diagnosis opens access to care and insurance coverage. Finally, it recognizes the biological impact of trauma, highlighting the measurable changes in the brain that require professional intervention.
Diagnostic and Statistical Manual of Mental Disorders research
PTSD: Mental Illness or Brain Injury?
Is PTSD a mental illness or a brain injury? It has elements of both. While not a physical injury like a concussion, trauma causes measurable changes to the brain. Research shows PTSD can lead to:
- A hyperactive amygdala (the fear center), causing heightened anxiety.
- A smaller hippocampus, affecting memory and emotional regulation.
- A less responsive prefrontal cortex, impairing decision-making.
Brain chemistry also changes, with imbalances in neurotransmitters like serotonin and cortisol. These biological changes demonstrate why PTSD is a complex condition impacting both mind and body, and why professional treatment is necessary for recovery.
What Causes PTSD? Who’s Most at Risk?
PTSD is caused by overwhelming traumatic events that shatter one’s sense of safety, not everyday stress. Not everyone who experiences trauma develops PTSD; it affects about 5% to 10% of those exposed.
![Diverse traumatic events. Alt text: “Common causes of PTSD: accident, disaster, violence”]
While some people’s brains process trauma and recover naturally, others have persistent symptoms that require support. Understanding the causes and risk factors can help you recognize when to seek help.
Common Causes
Any event that involves a serious threat can cause PTSD. Common causes include:
- Combat exposure
- Violent personal assaults (e.g., sexual assault, robbery)
- Childhood abuse or neglect, which can lead to complex PTSD and betrayal trauma
- Serious accidents, natural disasters, and life-threatening medical events
- Witnessing harm to others or learning about a trauma experienced by a loved one
Beginner’s Guide to Understanding Trauma
Risk Factors & Complications
Several factors increase the risk of developing PTSD, including prior trauma (especially in childhood), a lack of social support, genetics, and pre-existing mental health conditions. Women and members of marginalized groups are also at higher risk.
Left untreated, PTSD can lead to serious complications like co-occurring depression and anxiety, substance abuse, and chronic health problems. Most seriously, it significantly increases the risk of suicidal thoughts and attempts.
If you’re struggling with thoughts of suicide, call or text 988 for the Suicide & Crisis Lifeline. You are not alone.
Recognizing these risks isn’t about predicting doom—it’s about understanding when to seek help and knowing that recovery is possible.
How Is PTSD Treated? [Proven Therapies That Work]
PTSD recovery is not only possible but common. With treatment, about 70% of people recover completely or see significant improvement. Early intervention can even prevent PTSD from developing. Unlike conditions requiring lifelong management, PTSD can often be healed with the right trauma-focused approach.
Trauma-Focused Therapy
The most effective treatments are “trauma-focused therapies” designed to help your brain process traumatic memories. These include:
- Cognitive Processing Therapy (CPT): Challenges negative thoughts and beliefs caused by trauma.
- Prolonged Exposure (PE): Helps you gradually and safely face trauma-related memories and situations.
- Eye Movement Desensitization and Reprocessing (EMDR): Uses bilateral stimulation to help the brain reprocess “stuck” memories.
- Cognitive Behavioral Therapy (CBT): Provides skills to manage how thoughts, feelings, and behaviors are connected.
How EMDR Therapy Reduces PTSD Symptoms and Boosts Mental Health
The Benefits of CBT in Mental Health Treatment
Top 5 Effective Treatments for PTSD
Medications & Supportive Care
Medication can be crucial for managing severe symptoms, enabling you to engage in therapy. Antidepressants (SSRIs and SNRIs) like Zoloft and Paxil are FDA-approved for PTSD and help with mood and anxiety. Other medications can target specific symptoms like nightmares.
It’s important to know that medications manage symptoms but are not a cure. They provide stability for the healing work done in therapy, and a combination of both is often most effective.
Higher Levels of Care: Thrive’s IOP & PHP
When weekly therapy isn’t enough for severe PTSD, Intensive Outpatient Programs (IOP) and Partial Hospitalization Programs (PHP) offer more support. At Thrive Mental Health, our flexible virtual and hybrid IOP/PHP programs provide intensive, evidence-based care that fits your life.
These programs include structured group and individual therapy focused on building practical skills for managing triggers, regulating emotions, and improving communication. With virtual and evening options, you can access expert trauma care without putting your life on hold.
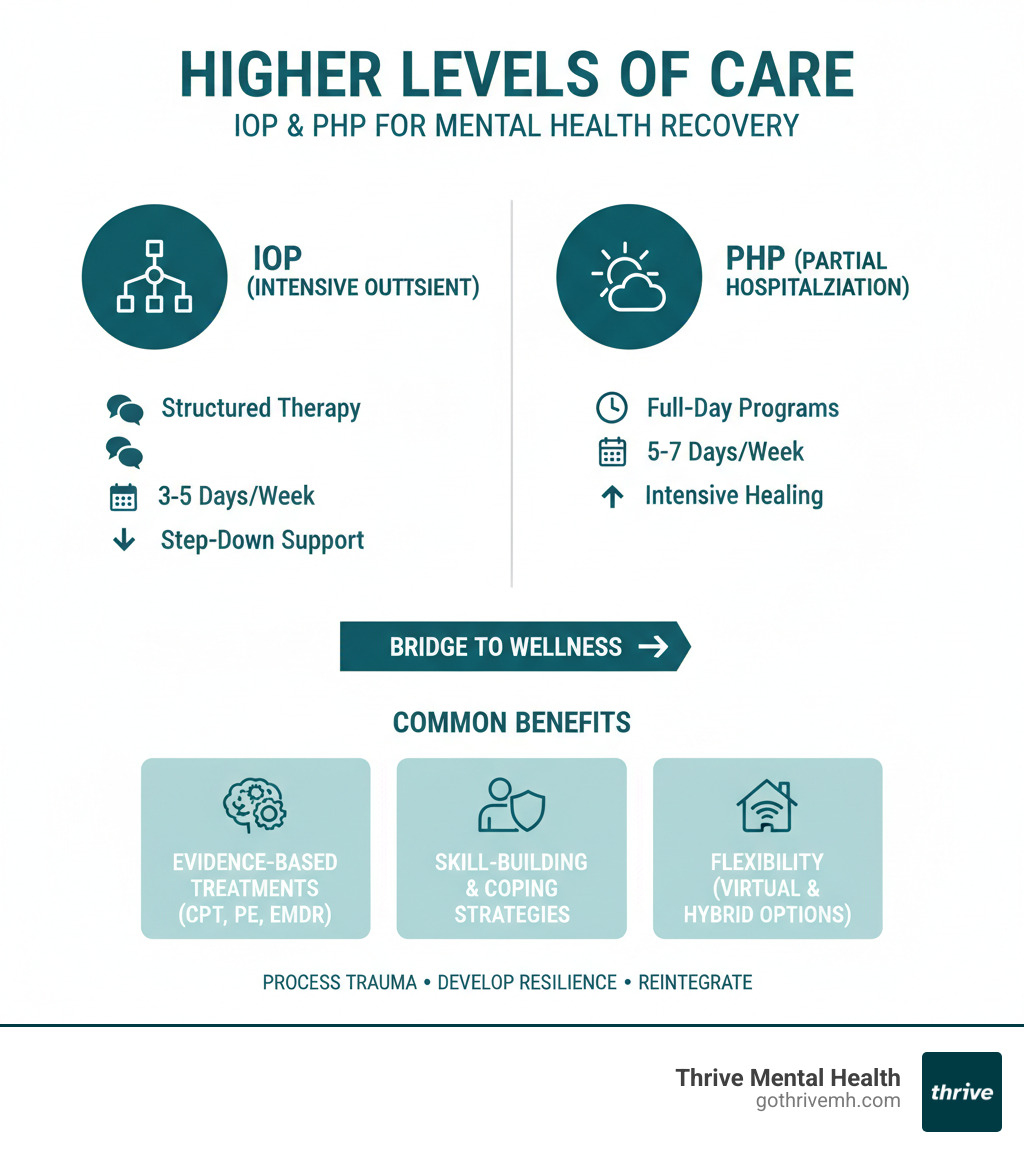
What Is the Difference Between PHP and IOP?
Thrive Virtual IOP & PHP Programs
Insurance Coverage for PTSD Treatment [Florida]
Because PTSD is a recognized mental illness, treatment is typically covered by insurance. At Thrive Mental Health, we work to remove financial barriers to care.
Most major insurance plans cover evidence-based PTSD treatment, including our virtual IOP/PHP programs. We are in-network with Cigna, Optum, Florida Blue, Aetna, UnitedHealthcare, and more.
Our team helps you steer your benefits. We’ll walk you through your coverage and explain any out-of-pocket costs upfront. Since coverage varies by plan, we offer a quick, no-obligation benefits check to clarify your coverage for our services in Florida.
Untreated PTSD is costly in terms of quality of life, which is why insurers cover effective treatments like IOP. Don’t let insurance confusion be a barrier; let our team help you maximize your benefits.
Verify Your Insurance in 2 Minutes
Medical Insurance Cover Therapy
Frequently Asked Questions about PTSD
Note for developers: Please implement JSON-LD FAQPage schema markup for this section.
Here are answers to common questions people have when they wonder, “is PTSD a mental illness?”
Can PTSD go away without treatment?
While acute stress reactions after trauma can fade, true PTSD rarely resolves on its own. The brain’s healing process gets stuck, and symptoms like flashbacks and hypervigilance often persist or worsen. Without professional help, people may develop unhealthy coping mechanisms. The good news is that PTSD responds very well to evidence-based treatment.
What’s the difference between PTSD and complex PTSD (C-PTSD)?
PTSD usually follows a single traumatic event, like an accident or assault. Complex PTSD (C-PTSD) stems from prolonged, repeated trauma, such as childhood abuse or domestic violence. C-PTSD includes all the symptoms of PTSD but also deeply affects one’s sense of self, emotional regulation, and ability to form healthy relationships. It requires specialized treatment to rebuild a stable sense of identity.
Does insurance cover PTSD treatment at Thrive?
Yes. Because PTSD is a recognized mental illness, insurance is required to cover evidence-based care. Thrive accepts most major insurance plans, including Cigna, Optum, Florida Blue, Aetna, and UnitedHealthcare. Our team can verify your specific benefits for our virtual IOP and PHP programs in Florida, so you know the costs upfront.
How do I start PTSD treatment at Thrive?
Starting is straightforward. You can call us directly at 561-203-6085 to speak with our compassionate team about your options. Alternatively, you can begin your benefits check on our website. We offer flexible virtual, hybrid, and evening programs to fit your life.
What if I’m in crisis or having suicidal thoughts?
If you are having thoughts of suicide, please call or text 988 immediately for the Suicide & Crisis Lifeline. This free, confidential service is available 24/7. PTSD can feel hopeless, but these crisis feelings are temporary. While waiting for support, stay with someone you trust and remove any means of self-harm. Your life is valuable, and recovery is possible.
Take the First Step: Hope and Healing Are Possible
The answer to “is PTSD a mental illness” is yes—and more importantly, it’s treatable. Your struggles are real, valid, and deserving of professional care. Recovery is possible with proven, evidence-based therapies.
![Diverse group in virtual therapy. Alt text: “PTSD treatment: virtual group therapy at Thrive Mental Health”]
You don’t have to wait to seek help; early intervention often leads to better outcomes. At Thrive Mental Health, we make starting treatment as easy as possible. Our flexible virtual and hybrid IOP/PHP programs in Florida, including evening options, are designed to fit your life.
Our trauma-focused care helps you process memories, regulate emotions, and reclaim your life in a supportive community. Our team handles the insurance verification, accepting most major plans. We’ll explain your coverage clearly before you commit.
Ready for support? Thrive offers virtual and hybrid IOP/PHP in Florida with evening options. Verify your insurance in 2 minutes (no obligation) → Start benefits check or call 561-203-6085. If you’re in crisis, call/text 988.