Complex Trauma Explained: How Therapy Can Help You Rebuild
Beyond a Single Event: Understanding Your Path to Healing
Therapy for complex trauma helps you heal from repeated or prolonged traumatic experiences—like childhood abuse, domestic violence, or ongoing neglect—that impact how you see yourself, relate to others, and steer daily life.
Quick Overview: What Makes Complex Trauma Different
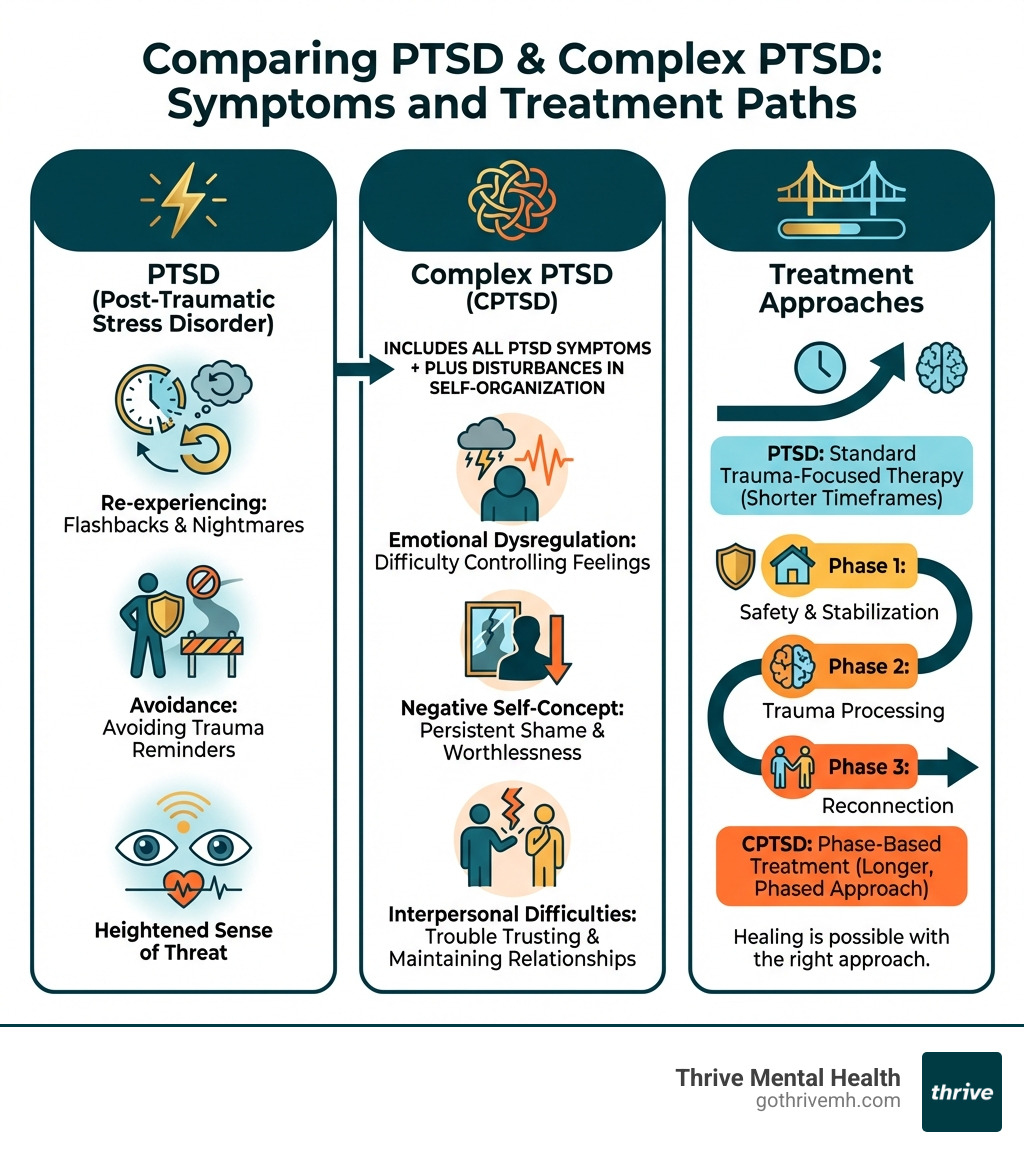
| Single-Incident Trauma (PTSD) | Complex Trauma (CPTSD) |
|---|---|
| One event (accident, assault) | Repeated or prolonged exposure |
| Flashbacks, nightmares, hypervigilance | All PTSD symptoms plus difficulty regulating emotions, negative self-image, relationship struggles |
| Standard trauma therapy often effective | Requires phased, longer-term treatment approach |
| Focus on processing the event | Focus on safety, identity rebuilding, and relational healing |
You might feel stuck in patterns you can’t explain: emotional outbursts, relationships that end the same way, or a persistent sense that something is wrong with you. These aren’t character flaws. They are adaptations your nervous system made to survive inescapable situations.
Research shows that experiencing trauma is remarkably common—but complex trauma is different because it happens repeatedly, often during childhood, and usually involves someone who was supposed to keep you safe.
The good news? Healing is absolutely possible. With the right therapeutic approach, you can rebuild your sense of safety, reclaim your identity, and create the relationships and life you deserve.
I’m Nate Raine, CEO of Thrive Mental Health. For the past decade, I’ve focused on making effective therapy for complex trauma accessible. Here in Florida, Thrive Mental Health provides innovative virtual and in-person care designed for driven professionals and young adults who need more structure than weekly therapy but with the flexibility to fit their lives.
What Is Complex PTSD? [The Hidden Wounds of Repeated Trauma]
Many people associate trauma with Post-Traumatic Stress Disorder (PTSD) from a single event like an accident or combat. But another form, Complex Post-Traumatic Stress Disorder (CPTSD), often goes unrecognized despite its pervasive impact. This is where specialized therapy for complex trauma becomes vital.
Unlike single-incident trauma, complex trauma stems from chronic, repetitive exposure to traumatic situations where escape was impossible. This includes childhood abuse or neglect, domestic violence, human trafficking, or prolonged exposure to war. These aren’t just events; they are inescapable conditions that fundamentally alter a person’s development and sense of self.
Betrayal trauma, a specific type of complex trauma, occurs when the abuse comes from someone the victim trusts and depends on, like a parent or partner. This shatters the victim’s sense of safety and ability to trust, making healing even more intricate. These hidden wounds are deep because they attack the very foundation of a person’s identity and their capacity for healthy relationships.

The Core Symptoms That Go Deeper Than PTSD
While CPTSD shares some symptoms with traditional PTSD—like re-experiencing events, avoidance, and hypervigilance—it also includes a distinct cluster of symptoms known as Disturbances in Self-Organization (DSO). These are the hallmarks that make CPTSD particularly challenging and require a specialized approach to therapy for complex trauma.
DSO manifests in several key ways:
- Emotional Dysregulation: Extreme difficulty controlling feelings, leading to intense mood swings, from explosive anger to deep despair. This can make everyday situations feel overwhelming.
- Negative Self-Concept: A persistent sense of shame, guilt, and worthlessness. You might feel fundamentally flawed or “bad,” often blaming yourself for the abuse you endured.
- Interpersonal Difficulties: Trusting others can feel impossible. You might struggle with forming healthy attachments, fear abandonment, or find yourself in cycles of unhealthy relationships, leading to profound loneliness.
- Dissociation: A coping mechanism where your mind “checks out” to protect itself from overwhelming pain. It can range from feeling detached from your body to experiencing memory gaps.
Understanding these deeper symptoms is crucial for effective treatment. If you’re struggling, know that you’re not alone. For a broader understanding of trauma, you can explore Understanding Post Traumatic Stress Disorder Symptoms, Causes, and Treatment Options.
Common Causes and Risk Factors
The roots of complex trauma are often found in repeated, prolonged exposure to traumatic stressors, many of which are Adverse Childhood Experiences (ACEs). ACEs are traumatic events that occur before age 18, such as:
- Abuse: Physical, emotional, or sexual abuse.
- Neglect: Physical or emotional neglect.
- Household Dysfunction: Growing up with domestic violence, substance abuse, mental illness, parental separation, or an incarcerated household member.
Watch a video on Adverse Childhood Experiences (ACEs) to understand their profound long-term impact.
Other chronic trauma exposures can also lead to CPTSD:
- Domestic Violence: Ongoing abuse within an intimate relationship.
- Emotional Incest: Blurred parent-child boundaries where the child meets the parent’s emotional needs.
- Narcissistic Abuse: Prolonged emotional manipulation, gaslighting, and control.
- War or Community Violence: Sustained exposure to violence.
- Human Trafficking: Being held captive and exploited.
Developmental trauma, which occurs during critical periods of brain development in childhood, often has a more profound impact on a person’s core identity and emotional regulation than adult-onset trauma. This is why therapy for complex trauma often requires a developmental lens. If you’ve experienced trauma in your formative years, read Overcoming Childhood Trauma: Healing Into Adulthood for more insights.
Why CPTSD Is Often Misdiagnosed (And How It Differs from BPD)
A major challenge in healing from complex trauma is getting an accurate diagnosis. CPTSD is recognized in the World Health Organization’s ICD-11 but is not yet a distinct diagnosis in the American Psychiatric Association’s DSM-5. This gap often leads to misdiagnosis or underdiagnosis, leaving many without the targeted therapy for complex trauma they need.

Without a specific CPTSD diagnosis, symptoms are often attributed to other conditions like depression, anxiety, or substance use disorders, and the underlying trauma goes unaddressed. A comprehensive assessment by a trauma-informed professional is critical. Our team at Thrive Mental Health in Florida understands these nuances and can provide the clarity you need to move forward. You can learn more in our article on Complex Post Traumatic Stress Disorder.
CPTSD vs. Borderline Personality Disorder (BPD)
The symptom overlap between CPTSD and Borderline Personality Disorder (BPD) is a primary reason for misdiagnosis. Both can involve:
- Impulsive behavior
- Fear of abandonment
- Unstable sense of self
- Emotional dysregulation
- Difficult relationships
However, the key difference is the root cause. CPTSD specifically requires a history of prolonged, repeated trauma, usually interpersonal and inescapable. The symptoms are adaptations to a traumatic environment. While trauma is often a factor in BPD, it is not a diagnostic requirement, and the underlying dynamics differ.
This distinction is vital because the treatment approach must be custom. For example, while Dialectical Behavior Therapy (DBT) is effective for both, how trauma processing is integrated might differ. If you’re interested in related therapeutic approaches, our MBT for BPD Guide may be insightful.
Specific Challenges in Therapy for Complex Trauma
Effective therapy for complex trauma requires navigating unique challenges with skill and patience:
- Building Trust: Survivors, especially those with betrayal trauma, often struggle to trust others, including therapists. Establishing a safe and consistent therapeutic relationship is paramount and takes time.
- Managing Dissociation: Therapists must be skilled in recognizing and gently addressing dissociation, helping clients stay grounded without becoming overwhelmed.
- Pacing Treatment: Rushing into trauma processing can be re-traumatizing. The pace must be carefully managed, ensuring clients have sufficient coping skills first.
- Addressing Attachment Wounds: Therapy must help clients understand their attachment patterns and develop healthier ways of relating to themselves and others.
- Slower Progress vs. PTSD Treatment: Healing from complex trauma often progresses more slowly than for single-incident PTSD. Research shows that individuals with a history of childhood trauma often benefit less from standard PTSD therapies, highlighting the need for specialized approaches.
Your Roadmap to Recovery: Evidence-Based Therapy for Complex Trauma
Healing from complex trauma is a journey, not a quick fix, requiring a structured, evidence-based roadmap. The good news is that specialized therapy for complex trauma is highly effective. Experts largely agree on a phase-based treatment model, with 84% endorsing this sequential approach. This model recognizes that diving into trauma memories without adequate preparation can be counterproductive.
The three phases of trauma treatment are:
- Stabilization (Safety and Skill-Building): Focusing on establishing safety, regulating emotions, and building coping resources.
- Trauma Processing (Remembrance and Mourning): Gently and safely processing traumatic memories and grieving losses.
- Integration (Reconnection and Rebuilding): Integrating the trauma experience into one’s life narrative and rebuilding a meaningful life.
This phased approach is backed by research and designed to create a solid foundation for healing. To learn more about the science behind effective trauma care, refer to Evidence-Based Trauma Treatment. For a deeper dive, a comprehensive review can be found in Complex PTSD: assessment and treatment.
Phase 1: Building Safety and Stability
Before addressing the deep wounds of trauma, we must establish safety and provide tools to manage overwhelming emotions. This initial phase of therapy for complex trauma is foundational and critical.
Key components include:
- Safety: Ensuring your current environment is physically and emotionally safe.
- Grounding Techniques: Learning practical strategies to return to the present moment when triggered.
- Emotional Regulation Skills: Developing the ability to manage intense emotions without being overwhelmed.
- Psychoeducation: Understanding how complex trauma affects your brain and body.
- Building the Therapeutic Relationship: Establishing trust with your therapist in a safe space.
Therapies that are particularly effective in this phase include:
- Dialectical Behavior Therapy (DBT): Highly effective for emotional dysregulation and distress tolerance. Read more about Dialectical Behavior Therapy.
- Somatic Therapy: Focuses on the body’s sensations to release stored tension and regulate the nervous system. Learn about the benefits of somatic therapy.
- Mindfulness: Practices that teach you to observe thoughts and feelings without judgment.
Research on stabilization therapies shows they significantly reduce symptoms, setting the stage for deeper trauma work.
Phase 2 & 3: Processing Trauma and Reconnecting with Life
Once a foundation of safety is established, Phase 2 involves gently processing traumatic memories—not to relive them, but to reduce their power over your present. This phase also involves grieving the losses associated with the trauma.
Phase 3 focuses on reconnecting with yourself and others, rebuilding a life of meaning, and integrating your healing into daily existence.
Several therapeutic modalities are highly effective in these phases of therapy for complex trauma:
- Eye Movement Desensitization and Reprocessing (EMDR): Helps the brain reprocess distressing memories, reducing their emotional charge. Explore our EMDR Complete Guide and the benefits of emdr therapy.
- Cognitive Behavioral Therapy (CBT): Helps challenge negative thought patterns resulting from trauma.
- Somatic Experiencing (SE): A body-oriented therapy that helps release stored trauma from the nervous system. Often, a combination of Somatic Therapy vs. EMDR: Which is Right For You? is used.
- Internal Family Systems (IFS): Helps heal and integrate different “parts” of the self into a cohesive whole.
- Narrative Exposure Therapy (NET): Focuses on creating a coherent life narrative that integrates traumatic events.
These modalities, applied within a phase-based framework, offer powerful pathways to reclaiming your life.
Individual vs. Group Therapy for Complex Trauma
Both individual and group therapy for complex trauma offer distinct benefits, and a combination is often most effective.
Individual Therapy: Provides a confidential, one-on-one space to build trust, process sensitive memories at a personal pace, and heal attachment wounds through the therapeutic relationship.
Group Therapy: Offers unique advantages for relational healing.
- Relational Healing: A safe environment to practice new ways of relating to others.
- Reducing Isolation: Fosters a sense of belonging and shared experience, combating the profound loneliness of trauma.
- Learning from Others: Witnessing others’ healing journeys can be empowering and provide new perspectives.
At Thrive Mental Health, our Virtual Group Therapy Sessions are available to residents across Florida, offering a supportive environment for relational healing to complement intensive individual work.
Are You Ready to Heal? [Preparing for Your Therapy Journey]
Starting therapy for complex trauma is a courageous step that requires readiness, not just a desire for change. Assessing your readiness helps ensure you are prepared for the work ahead and can maximize your healing.
Consider these factors:
- Life Stability: Is your living situation relatively stable and safe?
- Motivation: Are you genuinely motivated to engage in the hard work of healing?
- Support System: Do you have at least one trusted person for support outside of therapy?
- Coping Skills: Do you have some basic ways to manage stress? (If not, therapy will help you build them.)
It is completely okay if you do not feel “perfectly ready.” Part of therapy is developing these resources. For more insights, explore our Expert Tips on Coping with Trauma for Better Mental Health.
Self-Help Strategies to Start Today
While professional therapy for complex trauma is essential for deep healing, self-help strategies can support your journey. These practices build resilience, regulate your nervous system, and foster a stronger sense of self.
Here are some strategies to consider:
- Mindfulness Practices: Simple breathing exercises or body scans can help you stay present.
- Grounding Exercises: Use the 5-4-3-2-1 method (naming 5 things you see, 4 you touch, etc.) to anchor yourself in the present.
- Journaling: Writing down thoughts and feelings can be a powerful way to process emotions. You can Download a self-care diary to get started.
- Creative Expression: Art, music, or dance can provide a non-verbal outlet for difficult emotions. Learn more about Art Therapy for Trauma Recovery.
- Building a Routine: A predictable daily schedule can create a sense of stability and control.
- Reducing Avoidance: Gradually and safely re-engaging with things you have been avoiding can help you reclaim parts of your life.
These strategies are powerful allies in your healing process, not substitutes for professional therapy.
What to Expect: Goals and Outcomes of Therapy for Complex Trauma
Starting therapy for complex trauma is an investment in your future. While the journey is unique, you can expect common goals and transformative outcomes.
The primary goals include:
- Reduced Symptoms: A significant decrease in emotional dysregulation, flashbacks, dissociation, and hypervigilance.
- Improved Relationships: Developing healthier attachment patterns and fostering more fulfilling connections.
- Stronger Sense of Self: Moving from a negative self-concept to a more compassionate and authentic identity.
- Increased Emotional Regulation: Gaining greater control over your emotions and resilience.
- Greater Life Satisfaction: Experiencing more joy, purpose, and engagement in daily life.
Treatment Duration: Healing from complex trauma is a marathon, not a sprint. The initial phases of therapy for complex trauma (stabilization and processing) often take 9-12 months to show substantial benefits. Those with severe symptoms may need longer-term support over several years. Approach this journey with patience and self-compassion, and honor each step you take toward healing, no matter how small it may seem.
Frequently Asked Questions about Complex Trauma Therapy
What is the best therapy for complex trauma?
There is no single “best” therapy; effective treatment is often multi-component and phase-based. An expert consensus endorses a sequenced approach starting with stabilization (using skills from DBT, Somatic Therapy) followed by trauma processing (like EMDR or trauma-focused CBT). The right therapy depends on your specific symptoms and needs, and a trauma-informed therapist can help tailor the approach.
How long does it take to recover from complex PTSD?
Recovery is not linear and varies for everyone. Research suggests that structured programs lasting 9-12 months can lead to substantial benefits for the first two phases of treatment (stabilization and processing). However, individuals with severe symptoms and extensive relational ruptures may need intermittent support over several years to fully integrate healing and rebuild their lives.
Can you heal from complex trauma without therapy?
While self-help strategies like mindfulness and building a support system are beneficial, the deep-seated nature of complex trauma often requires professional guidance. A trauma-informed therapist provides the safety, structure, and specialized techniques needed to process traumatic memories and heal attachment wounds, which is very difficult to achieve alone. Therapy offers a unique environment for corrective emotional experiences that are hard to replicate independently.
Take the Next Step with Structured, Flexible Care in Florida
At Thrive Mental Health, we understand the courage it takes to seek help for complex trauma. We specialize in providing evidence-based therapy for complex trauma to residents throughout Florida. Our virtual and in-person Intensive Outpatient (IOP) and Partial Hospitalization (PHP) programs are designed for professionals and young adults needing structured healing that fits their lives.
With flexible virtual options and convenient in-person locations, we make specialized care accessible across the state. Our mission is to deliver measurable results, helping you rebuild your life with confidence. We work with major insurance providers, including Florida Blue, Aetna, Cigna, and UnitedHealthcare, to make care affordable. Learn more about our Florida-based Intensive Outpatient Programs.
Ready for support? Thrive offers virtual and hybrid IOP/PHP programs with evening options for Florida residents. Verify your insurance in 2 minutes (no obligation) → Start benefits check or call 561-203-6085. If you’re in crisis, call/text 988.