Unmasking COVID-19: Your Essential Guide to the Pandemic
The Real Risks of COVID-19 [And How to Protect Yourself]
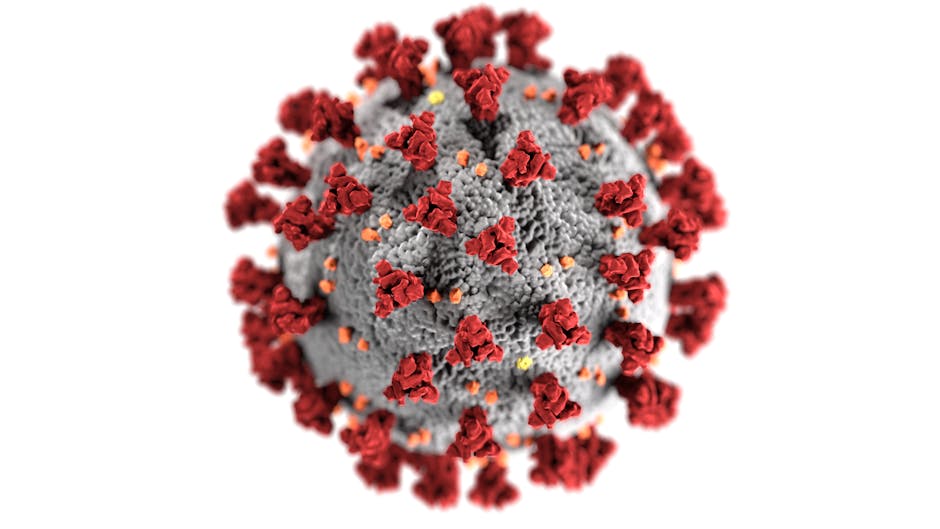
COVID-19 is the infectious disease caused by the SARS-CoV-2 virus that turned our world upside down. While the global emergency has passed, the virus remains a serious threat to your health and well-being. Understanding its risks is the first step to taking control.
Quick Facts About COVID-19:
- Caused by: SARS-CoV-2, a coronavirus
- Symptoms: Fever, cough, shortness of breath, fatigue, loss of taste/smell (appear 2-14 days after exposure)
- Severity: 81% mild/moderate, 14% severe, 5% critical
- Transmission: Respiratory droplets, airborne particles, close contact
- Contagious Period: Up to 2 days before symptoms + 10-20 days after
- Complications: Respiratory failure, organ damage, long COVID (persistent symptoms lasting weeks to months)
- Prevention: Vaccination, hand hygiene, masks in high-risk settings, testing when symptomatic
The pandemic has claimed over 7 million reported lives worldwide, with the actual toll estimated to be far higher. But the danger isn’t just mortality. Up to 44% of infected people show no symptoms at all, yet they can unknowingly spread the virus to vulnerable loved ones. Others are left battling debilitating symptoms for months after the initial infection clears.
The mental health impact has been just as severe. The trauma of isolation, loss, and chronic illness has fueled a crisis of anxiety, depression, and burnout—especially among professionals and young adults.
As CEO of Thrive Mental Health, I’ve seen how COVID-19 has exposed the urgent need for accessible mental health care. We’ve built virtual and hybrid programs across Florida to help people recover from both the immediate and lasting impacts of the pandemic.

Learn more about covid-19:
How You Catch COVID-19 (Even When You Feel Safe)
COVID-19 is the disease caused by SARS-CoV-2, a coronavirus that spreads with alarming efficiency. First identified in late 2019, it was declared a pandemic on March 11, 2020. While the global emergency status was lifted on May 5, 2023, the virus continues to circulate and evolve, posing an ongoing risk.
The primary way COVID-19 spreads is from person to person. When an infected individual breathes, talks, or even laughs, they release tiny infectious particles into the air. You can become infected by inhaling these particles. This airborne transmission is a major risk in indoor spaces with poor ventilation, where the virus can linger and accumulate.
Understanding the infection timeline is key to protecting yourself and others. After exposure, symptoms can take anywhere from two to 14 days to appear (the incubation period). The most dangerous part? An infected person can spread the virus for up to two days before they feel sick. They remain contagious for 10 to 20 days after symptoms start. This means you can unknowingly spread the virus to colleagues, friends, and family, making preventative measures absolutely critical.

What are the common symptoms of COVID-19?
Symptoms of COVID-19 range from non-existent to severe. Even if you feel fine, you could be contagious. The most common signs of infection include:
- Fever or chills
- Cough
- Shortness of breath or difficulty breathing
- Fatigue
- Muscle or body aches
- Headache
- New loss of taste or smell
- Sore throat
- Congestion or runny nose
- Nausea or vomiting
- Diarrhea
Mild cases may last a week or two, but severe illness can drag on for months. Shockingly, research suggests up to 44% of infected people remain completely asymptomatic. These silent carriers are a major reason why community-wide prevention is so vital.

How is the severity of a COVID-19 illness classified?
COVID-19 impacts people differently. Healthcare providers classify its severity to determine the right level of care:
- Mild to Moderate Illness: About 81% of people fall into this category. They experience symptoms like fever, cough, and fatigue but don’t have significant breathing trouble. Most can recover at home.
- Severe Illness: Roughly 14% of individuals develop severe symptoms, including shortness of breath (dyspnea) and low blood oxygen (hypoxia). This stage often requires hospitalization.
- Critical Illness: Around 5% of patients face life-threatening conditions like respiratory failure, septic shock, or multi-organ dysfunction. These cases require intensive care and mechanical ventilation.
Know the warning signs. If you or someone else experiences severe shortness of breath, persistent chest pain, new confusion, or bluish lips, call 911 immediately. For more details, refer to trusted medical guides like this one: More on COVID-19 symptoms and causes from Mayo Clinic.
Beyond the Cough: Severe Illness, Complications, and Long COVID
While most people recover from COVID-19, the virus can cause severe, life-altering illness, especially for those with certain risk factors. Your risk of hospitalization and severe outcomes increases significantly if you are:
- An Older Adult (65+): Age remains a primary risk factor for severe disease.
- Living with Chronic Conditions: Heart disease, diabetes, chronic lung or kidney disease, and obesity make you more vulnerable.
- Immunocompromised: A weakened immune system from conditions like cancer or certain medications puts you at higher risk.
- Pregnant: Pregnancy increases the risk of severe COVID-19 and can lead to adverse outcomes.
These factors explain why the virus can overwhelm the body, leading to hospitalization and the need for intensive care.
What are the potential complications of a COVID-19 infection?
A COVID-19 infection can inflict damage far beyond your lungs, attacking multiple organ systems with devastating results. Potential complications include:
- Respiratory Failure and Lung Damage: Severe cases can lead to acute respiratory distress syndrome (ARDS) and permanent lung scarring.
- Heart Muscle Damage: The virus can injure the heart (myocarditis), leading to heart failure or arrhythmias.
- Kidney Injury: Up to 30% of hospitalized patients suffer kidney damage, sometimes requiring dialysis.
- Liver Injury: Liftd liver enzymes, a sign of liver injury, are seen in 20-30% of people with COVID-19.
- Nervous System Problems: Complications range from loss of smell to strokes, seizures, and brain inflammation.
- Blood Clots: The infection raises the risk of dangerous blood clots that can cause a pulmonary embolism, heart attack, or stroke.
- Multisystem Inflammatory Syndrome (MIS-C/MIS-A): A rare but serious condition where various body parts become inflamed, affecting both children and adults weeks after infection.
The Lingering Shadow: Understanding Post-COVID-19 Syndrome
For many, the battle doesn’t end when the infection clears. Post-COVID-19 Syndrome, or “Long COVID,” leaves individuals with persistent or new symptoms for months, regardless of the initial illness’s severity. It’s a chronic condition that can shatter your quality of life.
Common symptoms include:
- Profound Fatigue: A bone-deep exhaustion that rest doesn’t fix.
- Brain Fog: Crippling difficulties with memory, focus, and thinking clearly.
- Shortness of Breath: Ongoing breathing problems, even with minimal effort.
- Muscle and Joint Pain: Persistent, widespread aches.
- Heart Palpitations: A racing or fluttering heartbeat.
- Sleep Disturbances: Insomnia and other sleep issues.
The mental toll of Long COVID is immense. The constant physical symptoms and uncertainty fuel anxiety, depression, and PTSD, making it hard to work, maintain relationships, or feel like yourself again. This is where targeted support becomes essential.
At Thrive Mental Health, we understand the pandemic’s deep and lasting mental health consequences. Our expert-led virtual programs are designed to help you manage the anxiety, depression, and trauma that come with conditions like Long COVID. Learn about virtual mental healthcare for complex needs and start your journey toward recovery.
Your Defense Plan: Testing, Prevention, and Navigating Variants
Fighting COVID-19 requires a smart, multi-layered defense. Knowing your testing options and sticking to proven prevention strategies gives you the power to protect yourself and those around you.
| Test Type | Accuracy | Speed of Results | Best Use Case |
|---|---|---|---|
| PCR Test | Highly accurate (detects viral RNA) | Hours to days | Confirming infection, especially with symptoms |
| Rapid Antigen | Less sensitive than PCR (detects viral proteins) | ~15 minutes | Quick screening, before events/travel, with symptoms |
| Antibody Test | Detects past infection (antibodies) | Days | Assessing previous exposure, not current infection |
Your strongest tools against the spread of COVID-19 are consistent prevention habits:
- Vaccination: Staying up-to-date on COVID-19 vaccines is the single most effective way to prevent severe illness, hospitalization, and death.
- Hand Hygiene: Wash your hands with soap and water for at least 20 seconds. When that’s not possible, use a hand sanitizer with at least 60% alcohol.
- Masks: Wear a high-quality, well-fitting mask in crowded indoor settings, especially if you or someone you’re with is at high risk.
- Physical Distancing: Keep a safe distance from others in crowded areas, particularly those with poor airflow.
- Improving Ventilation: Open windows, use fans, or run an air purifier to disperse virus particles indoors.
How is COVID-19 diagnosed and what tests are available?
Diagnosing COVID-19 involves a viral test for a current infection or an antibody test for a past one.
- Viral Tests: These look for the SARS-CoV-2 virus itself.
- PCR (Polymerase Chain Reaction) Tests: Considered the “gold standard” for accuracy, these lab tests detect the virus’s genetic material. Results can take hours to days.
- Rapid Antigen Tests: These at-home tests provide results in about 15 minutes by detecting viral proteins. They are less sensitive than PCR tests and may miss some infections, particularly if you’re asymptomatic.
- Antibody Tests: These blood tests identify antibodies from a past infection or vaccination. They cannot diagnose a current infection, as it takes at least 12 days for antibodies to develop.
Test if you have symptoms, were exposed to someone with COVID-19, or before gathering with vulnerable people. For local testing information, residents in Florida can find the most current guidelines on their county health department website or the official Florida Department of Health site.
Staying Ahead of the Virus: Vaccines and Variants
The SARS-CoV-2 virus is constantly mutating, leading to new variants. Some variants are more concerning because they can:
- Spread Faster: Increased transmissibility leads to rapid outbreaks.
- Cause More Severe Illness: Some variants may lead to worse outcomes.
- Evade Immunity: Mutations can make the virus better at bypassing protection from past infection or vaccination.
Staying up-to-date on your vaccinations is our best defense. Updated vaccines are designed to target the most common variants, providing robust protection against severe disease. Even if you’ve had COVID-19, vaccination is recommended to build a broader and more durable immune response.
As you steer these complexities, mental resilience is key. Our Partial Hospitalization Program (PHP) provides structured support for those needing intensive mental health care. Explore our Partial Hospitalization Program (PHP) to see how we can help you build the skills to cope and thrive.
Frequently Asked Questions about COVID-19
How long is someone contagious with COVID-19?
A person infected with COVID-19 can be contagious up to two days before symptoms appear. They typically remain contagious for 10 to 20 days after symptom onset, depending on the severity of their illness. Individuals who never develop noticeable symptoms (asymptomatic carriers) can still spread the virus to others.
Can you get COVID-19 more than once?
Yes, reinfection with COVID-19 is possible. As the virus mutates and new variants emerge, prior infection may not provide complete or long-lasting protection against different strains. While previous infection offers some natural immunity, it can wane over time, and getting vaccinated even after infection helps boost and broaden your immune response.
What should I do if I test positive for COVID-19?
If you test positive for COVID-19, you should immediately follow current public health guidelines for isolation in your area. This typically involves staying home and away from others to prevent further spread. Rest, stay hydrated, and monitor your symptoms closely. If your symptoms worsen, or if you are at high risk for severe disease due to age or underlying health conditions, contact a healthcare provider promptly. They can advise on potential treatments or further steps.
Conclusion: Navigating the New Normal with Confidence
The COVID-19 pandemic has changed our world, but it remains a significant health threat that demands your attention. Understanding the virus, its risks, and your prevention options is the key to protecting yourself and your community. From recognizing symptoms and transmission to preparing for severe complications and the effects of Long COVID, knowledge empowers you to make decisions that safeguard your well-being.
Crucially, the pandemic has proven that physical and mental health are inseparable. Managing the long-term mental health fallout is a critical part of recovery. At Thrive Mental Health, we are committed to helping you through these challenges. We provide expert-led virtual and hybrid programs across Florida, offering a lifeline for adults struggling with anxiety, depression, and other conditions exacerbated by the pandemic. Our programs, often covered by major insurers like Cigna, Optum, and Florida Blue, make evidence-based care accessible, helping you steer the new normal with strength and confidence.
Ready for support? Thrive offers virtual and hybrid IOP/PHP programs with evening options. Verify your insurance in 2 minutes (no obligation) → Start benefits check. If you’re in crisis, call/text 988.